Sacroiliac Joint Displacement Causes “Leg Length Discrepancy”, Upper Cervical (C0-C2) Deviation, Sympathetic Autonomic Hyperactivity, & Widespread Neurophysiologic Destruction (and why Heel Lifts Suck)
The only instance where heel lifts make sense, to me, is if you are dealing with a toe walking patient secondary to cerebral palsy or some other underlying neurologic impairment. The overwhelming majority of the time heel lifts are given to patients by physical therapists, it is because the patient has come to physical therapy with the diagnoses of a “leg length discrepancy.” The problem with this is, a minute percentage of people diagnosed with a “leg length discrepancy” actually have a difference in the length of their legs. Treating a problem that does not exist fixes nothing, and oftentimes makes things worse. If the patient actually does have a leg length discrepancy, which is rare, heel lifts still make no sense. Why would you ever want to elevate one heel? Their other heel is not elevated. All this does is lead to contractures of the posterior leg muscles and pathology throughout the spine. If a true leg length discrepancy is present, a full shoe lift makes sense. Heel lifts don’t, and they suck.
There are only a few ways people develop a true leg length discrepancy. Breaking a growth plate during adolescence without proper treatment, poor surgery leading to altered joint position, or congenital deficits, such as Legg-Calve-Perthes disease. If none of these factors are present, it is almost certain your patient does not have a leg length discrepancy. The only objective way to determine a true leg length discrepancy is to measure the femur and tibia on X-rays. I can tell you from 10 years of clinical practice, I have received two diagnoses of this condition that have actually been objectively measured and confirmed. Not coincidentally, these were the only two cases of actual leg length discrepancy I have seen. Most medical practitioners in the US have decided to completely disregard the concept of critical thinking, and most of them are super happy this way. If there is no reason the legs should be different lengths, what is the other obvious thing that could alter this? Hint: it’s not aliens. Do you ever hear about any other bones in our body randomly and significantly losing symmetry? Does one side of your face grow longer than the other? Arms different lengths? No? So, why in the world would the assumption for the legs be in complete opposition to all other bones in the body? If someone comes in with a shoulder problem, do you tell your patient they are basically screwed because their arms must be different lengths? No, you don’t. You treat the joints, muscles, and other soft tissues in the shoulder and throughout the body. Why is the thinking about the leg so contradictory and nonsensical?
The SIJ’s should not move a whole lot. However, they move, and move way more than most medical doctors understand. In women, especially during and after pregnancy, The SIJ’s move quite a bit, secondary to relaxin and other substances that loosen ligaments to facilitate childbirth. Although the sacroiliac joints do not move nearly as easily in men, once they get deviated, they often cause more of a problem than in women, precisely because they are more stable. Typically, the more stable the joint, the more noticeable it is when deviated. Unfortunately for both sexes, most medical practitioners believe there is no fix for supposed “leg length discrepancies”, which they assume to be the problem, without ever checking to see if it is an impairment or not. So, if you are having low back pain, hip pain, sacroiliac pain, headaches, or whatever, and your legs appear different in length, which they do in most people suffering from these conditions, you automatically get put into the “leg length discrepancy” basket. This ensures you will never get better, because all thinking has stopped, if it ever occurred in the first place. If you have been diagnosed with a problem you don’t have, then given a heel lift to abnormally elevate one heel to try to fix a problem that is not there, nothing good happens.
Osteokinematic Movement of the Sacroiliac Joints in Relation to the Legs
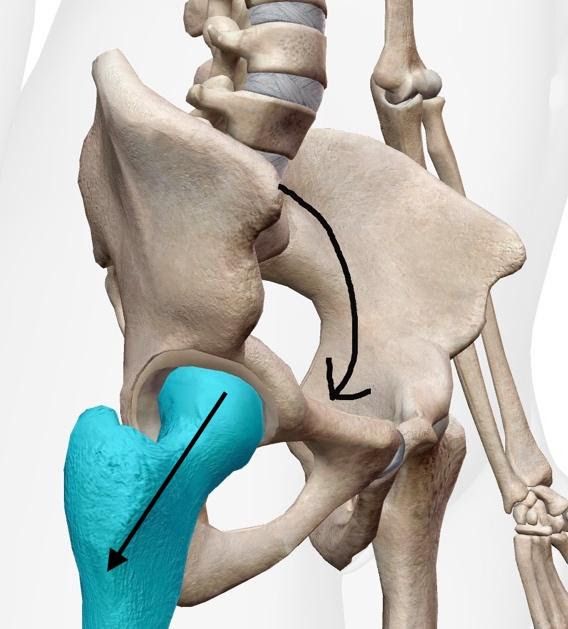


Structurally speaking, it is easiest for the ilium to get displaced into anterior rotation and/or medial rotation, in relation to the sacrum. When the ilium goes into anterior rotation, it pushes the acetabulum toward your feet, making that leg appear longer. This is just how the pelvis moves. The sacrum is a wedge, like the top piece of an arch. If the ilium rotates posteriorly and/or externally, the ilial joint line jams into the sacral joint line, and the wedge shape of the sacroiliac joint typically limits significant deviation. It is certainly possible for the ilium to deviate into posterior and/or external rotation, but this is only common if you get run over by an NFL linebacker, get into a car accident, step into a hole you did not know was there, or something like that. The architecture of the sacroiliac joints makes random deviation into these directions unlikely.
There are only 3 true pelvic joints; the symphysis and the two sacroiliac joints. This should make the pelvis easy to assess. The problem is the way people are taught to assess the pelvis, which assumes so many things it cannot possibly be specific, sensitive, accurate, or precise. We were all taught to look at the anterior and posterior sacroiliac spines in standing, sitting, prone, supine, bla, bla, bla. Assessing the pelvic joints this way assumes equal length, tonicity, fluid saturation, etc., of all the muscles attaching to the pelvis on the left and right. Anyone have patients who present with the exact same soft tissue status on the left and right sides of their body? By looking at the pelvis in different patient positions, you are massively changing the forces being transmitted through the pelvis from the muscle, tendon, and ligamentous attachments. If anything, looking at the pelvis in different patient positions tells you more about the muscles than the joints. You mean completely disregard the standard of thinking and the standard of care for hip pathology we learned in school? Yes, that is precisely what I mean.
If you are assessing the pelvic joints, looking at the patient’s pelvis in different positions is a waste of time. It mentally paralyzes most practitioners, as it well should, because it makes no sense. Place the patient in supine and straighten them out on the table. Have them do a bridge with their hips and then extend their legs. I pull both legs equally to further straighten them out. Whatever leg looks longer, assume that side of the ilium is rotated anteriorly on the sacrum. We will deal with possible medial or external rotation of the ilium in a sec. So, if the ilium on the longer leg side is in anterior rotation, we need to push it into posterior rotation.
If performed properly, this will magically and immediately make one leg shrink! like Harry Potter… I mean, it will reduce the anteriorly rotated sacroiliac joint to neutral, and the legs will be the same length. Because the legs are almost never the problem!
Once I correct for anterior rotation, I look at the position of the anterior superior iliac spines, in relation to the belly button, with the patient in supine. If one side is closer to the belly button, I assume that ilium is rotated medially on the sacrum. So, I push it into external rotation. I like to do this one bilateral, as I think most people’s sacroiliac joints are bilaterally displaced into medial rotation (medial rotation of the ilium on sacrum). This is also a great lumbar manipulation. The lumbar spine must be addressed in all cases of “leg length discrepancy.”
Note: I like to needle prior to manipulating. This normalizes soft tissue, allows for better, more comfortable reduction of the joints, and allows for complexes, like the pelvis, to self-correct following joint manipulation.
If the ilium goes into too much anterior rotation, the posterior sacroiliac spine, along with the posterior superior sacroiliac ligament, push the L5 transverse process on that side, forward. So, if the right ilium goes too far anterior, it will push the backside of the L5 transverse process, turning the lumbar spine into left rotational deviation. If the lumbar spine gets pushed into left rotation, what is the easiest segment of our spine to compensate for rotational deviation throughout the spine? C1/C2 is the answer.
C1/C2 has about 40-45 degrees of rotation. The next biggest rotation, per segment, is also in the cervical spine, but it is less than 15 degrees. That means C1/C2 has 3 times the amount of rotation compared to the next most mobile segment, making it the easiest segment, mechanically, for our body to use to compensate for deviation elsewhere. This causes upper cervical spine / subcranial spine deviation. This is bad.
Here are some illustrations of issues that arise from pathology in the upper cervical spine:

Trigeminocervical nucleus (complex). Baron EP, Cherian N, Tepper SJ. Role of Greater Occipital Nerve Blocks and Trigger Point Injections for Patients with Dizziness and Headache. The Neurologist. 2011; Nov;17(6):312-7.

DOI: https://doi.org/10.1101/2022.01.04.22268756
Illustration of the dorsal aspect of the cervicomedullary junction, depicting the lesion site for nucleus caudalis interventions including DREZ nucleotomy/tractotomy, percutaneous nucleotomy/tractotomy, and cervical SCS.
Abbreviations: DREZ, dorsal root entry zone; SCS, spinal cord stimulation.

DOI: 10.1152/physrev.00034.2015

DOI: 10.1152/physrev.00034.2015
Caption
FIGURE 9. Anatomy and pharmacology of the hypothalamic nuclei and brain stem nuclei involved in energy homeostasis and pain modulation in the context of migraine. Projections to and from specific nuclei within the hypothalamus are involved in the complex neural circuitry of energy homeostasis, including the arcuate (ARC), paraventricular (PVN), ventromedial (VMH), dorsomedial (DMH), and lateral (LH) hypothalamic neurons. In the ARC, energy homeostasis is controlled by orexigenic neuropeptides [stimulating () food intake and decrease energy expenditure] neuropeptide Y (NPY) and agouti-related peptide (AgRP) and anorexigenic peptides [inhibit () food intake and increase energy expenditure] proopiomelanocortin (POMC) and cocaine and amphetamineregulated transcript (CART). Peripheral circulating hormones insulin and leptin inhibit NPY/AgRP and stimulate POMC/CART neurons. Communication among these neural circuits is further controlled by the release of orexin A and B, corticotropin-releasing factor (CRF), melanin-concentrating hormone (MCH),-aminobutyric acid (GABA), glutamate (GLU), and brain-derived neurotrophic factor (BDNF), among others. The role these nuclei have in potentially triggering migraine, as a consequence of altered feeding and changes in energy homeostasis, is through their descending projections to brain stem nuclei known to be involved in the modulation of pain processing related to headache. These include direct PVN projections to the trigeminocervical complex (TCC), VMH projections to the periaqueductal grey (PAG) and the locus coeruleus (LC), and indirect communication through the ventral tegmental area (VTA) and nucleus tractus solitarius (NTS). Hypothetically altered feeding will affect neuronal processing in the ARC, and subsequently in other hypothalamic nuclei through its connections to them, including the PVN, VMH, and LH. Their control of transmission of nociceptive inputs to the trigeminovascular system may be altered, which ultimately produces the perception of noxious input from the craniofacial region and activation of trigeminovascular system, with a specific injury or insult. NPY1R and NPY5R, NPY receptors; OX1R and OX2R, orexin receptors; ObRb, long " signaling " isoform of the leptin receptor; INSR, insulin receptor; 3V, 3rd ventricle.
In the picture above with the full brain, the very bottom black dot labeled TCC is the trigeminocervical nucleus at C2. If C2 becomes deviated to compensate for sacroiliac displacement, now the two primary parasympathetic portions of the spinal cord are pathological, the sacral plexus (S2-S4), and the upper cervical spine (secondary to cranial nerves V, IX, X). Remember, in general, pathology anywhere in the body stimulates the sympathetic autonomic nervous system to elevate, which reciprocally inhibits, or depresses, the parasympathetic portion of the autonomic nervous system.
The primary nerve of the parasympathetic system is the vagus nerve, cranial nerve X. The vagus nerve is the connector between the gut and the brain (gut-brain axis), the adrenal glands and the brain (hypothalamic-pituitary-adrenal axis), and is the primary information highway between the rest of our organs and our brain. 80% of the vagus fibers are afferent, meaning the top priority of the vagus is to tell the brain what is going on with the organs, so the brain can process the information and respond by sending the necessary controlling stimuli. Another term is interoceptive awareness. If the sympathetic nervous system is hyperactive, as it is in the majority of humanity, the most negatively affected structure is going to be the most parasympathetic-dominant structure in the body – the vagus nerve.
The more parasympathetic the structure, the more inhibition secondary to sympathetic hyperactivity. Remember, sympathetic hyperactivity is the natural human response to mental and physical stress, strain, pain, and trauma. When the vagus is inhibited, the brain receives faulty information about the organs. Without proper information coming in, the brain is unable to send the correct regulating signals back to the organs. This can lead to about any physical or mental impairment you can think of, including cancer, dementia, tinnitus, hearing loss, neuropathy anywhere in the body, pain, brain fog, incontinence, erectile dysfunction, and a lot more bad stuff.
The trigeminal nerve, Cranial nerve V, is a nerve with strong parasympathetic ganglia in the brain. Many of the points of connection in the trigeminocervical complex intricately interconnect with the hypothalamic-pituitary-adrenal axis. If these axes start receiving hyperactive sympathetic stimulation, the concentrations of all our hormones, endogenous opioids, neuromodulators, etc., become abnormal. This is a reason why it is so important to always target parasympathetic portions of the autonomic nervous system, including the vagus nerve distribution in the ear, along with whatever else you are treating. This maximally stimulates parasympathetics, depresses sympathetics, and brings the autonomic nervous system toward homeostasis. Autonomic nervous system homeostasis is the key to health and longevity.
The goal of all medical treatment should be to put the autonomic nervous system in as much homeostasis as possible. If the autonomic nervous system goes over your individual threshold for sympathetic activity, it loses its ability to self-regulate. The brain and the body know how to work properly, in the vast majority of humans. The problem is, extrinsic factors like pathologic tissue and joints start sending enough pathologic afferent signals to the brain and start utilizing enough energy, where your autonomic system has no chance to recover the ability to self-regulate. This leads to all our systems becoming energy deficient. Our cells start producing less energy per molecule of glucose processed and our system runs out of energy. The mitochondria in the cells run out of ATP, NADH, and NAD+, then our systems have to decide where to send energy, because we no longer have enough to properly deal with everything going on. This is what leads to cancer, autoimmunity, diabetes, hearing loss, chronic pain, etc.
The trick is, figuring out how to put gas back in the generator, energy back in the battery. The best ways to do this are thoughtful dry needling combined with joint manipulation, along with consistent exercise, eating well, proper supplementation, and sleeping well. Unfortunately, most Americans do not do the last 4. If you need evidence of this, 40% of US citizens are obese, 67% are overweight, and 70% are vitamin D deficient. If you want some awesome information about why exercise, diet, and sleep are so important, check out Dr. Andrew Huberman (Huberman Lab Podcast) and Dr. Peter Attia (The Drive Podcast).
Every tiny piece of normalized soft tissue, every normalized joint, every millimeter of normalized capsular tissue, removes stress from the autonomic nervous system and gives energy back to it. If you restore enough energy to the autonomic nervous system, the mind and body break out of their inhibited state and once again become able to direct ample resources to fix ongoing problems. I think of it as running an antivirus program on the computer. Barring specific injury, almost all “idiopathic” impairments have a root cause of autonomic nervous system energy deficiency and a departure from homeostasis. Rather than trying to fix specific impairments, if we try to fix the autonomic nervous system, we allow the brain and body to fix themselves. Trust me, our systems know how to fix themselves far better than we ever will. We just need to remove the stuff inhibiting them from doing so.
DISCLAIMER: The content on the blog for Intricate Art Spine & Body Solutions, LLC is for educational and informational purposes only, and is not intended as medical advice. The information contained in this blog should not be used to diagnose, treat or prevent any disease or health illness. Any reliance you place on such information is therefore strictly at your own risk. Please consult with your physician or other qualified healthcare professional before acting on any information presented here.
References
- Goadsby, Peter & Holland, Philip & Martins-Oliveira, Margarida & Hoffmann, Jan & Schankin, Christoph & Akerman, Simon. (2017). Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiological Reviews. 97. 553-622. 10.1152/physrev.00034.2015.
- Surgical interventions targeting the nucleus caudalis for craniofacial pain: a systematic and historical review Brendan Santyr, Mohamad Abbass, Alan Chalil, Amirti Vivekanandan, Margaret Tindale, Nicholas M. Boulis, Jonathan C. Lau. medRxiv 2022.01.04.22268756; doi: https://doi.org/10.1101/2022.01.04.22268756
- Charbit, A.R., Akerman, S., Holland, P.R. and Goadsby, P.J., 2009. Neurons of the dopaminergic/calcitonin gene-related peptide A11 cell group modulate neuronal firing in the trigeminocervical complex: an electrophysiological and immunohistochemical study. Journal of Neuroscience, 29(40), pp.12532-12541.
- Qu, Z., Liu, L., Zhao, L., Xu, X., Li, Z., Zhu, Y., Zhang, C., Jing, X., Wang, X., Li, B. and Zhang, C.S., 2020. Prophylactic electroacupuncture on the upper cervical segments decreases neuronal discharges of the trigeminocervical complex in migraine-affected rats: an in vivo extracellular electrophysiological experiment. Journal of Pain Research, pp.25-37.
- Thoma, P., Drämel, N., Grothe, M., Lotze, M., Fleischmann, R. and Strauss, S., 2022. Impaired Pain Processing at a Brainstem Level Is Involved in Maladaptive Neuroplasticity in Patients with Chronic Complex Regional Pain Syndrome. International Journal of Molecular Sciences, 23(23), p.15368.
- Brandt, R.B., Ouwehand, R.L.H., Ferrari, M.D., Haan, J. and Fronczek, R., 2022. COVID-19 vaccination-triggered cluster headache episodes with frequent attacks. Cephalalgia, 42(13), pp.1420-1424.
- Liu, S., Wang, Z., Su, Y., Qi, L., Yang, W., Fu, M., Jing, X., Wang, Y. and Ma, Q., 2021. A neuroanatomical basis for electroacupuncture to drive the vagal–adrenal axis. Nature, 598(7882), pp.641-645.