To Piston or Not to Piston: Should I Utilize the “Pistoning” Technique When Performing Dry Needling?
Sympathetic-dominant autonomic nervous system (ANS) hyperactivity, fight-or-flight response, is only potentially beneficial for human well-being in short durations. A few minutes to a few days, at most. After that, chronic sympathetic autonomic hyperactivity becomes detrimental to all aspects of health. The natural response of the human mind and body to mental or physical stress, strain, pain, or trauma, is to elevate sympathetic activity. Therefore, almost all physical therapy patients present with chronic sympathetic hyperactivity. Almost all psychotherapy patients present this way as well. Most of humanity presents this way, for that matter. This is a massive problem that goes largely unaddressed. To counter this, it is necessary to remove as many sympathetic stressors from the joints and tissues throughout the body as possible, while concomitantly targeting the parasympathetic autonomic nervous system (PANS) to inhibit sympathetic activity and nudge the autonomic nervous system toward homeostasis, the key to health. A primary factor limiting the amount of treatment an individual can tolerate is how much sympathetic autonomic stimulation you induce while inserting needles.
Each time you get poked with a sharp piece of metal, the sympathetics are stimulated. The more pokes, the more sympathetic stimulation. The more sympathetic stimulation, the more likely you are to push your patient vasovagal. Needle-induced vasovagal response is secondary to sympathetics elevating too much, too fast, for the individual’s threshold, leading to a rapid increase in blood pressure. This stimulates the baroreceptors in the carotids, along with other neurophysiologic processes, and ignites the opposing part of the autonomic nervous system, the parasympathetic autonomic nervous system (PANS). The parasympathetics crank up to rapidly depress the sympathetics and protect the mind and body. This is an uncomfortable experience for patients, especially if the body overreacts to the point of induced fainting. I have never had a patient lose consciousness. Targeting the vagus nerve with your first needles helps avoid this as it regulates the autonomic nervous system toward homeostasis.
Remember, the vagus nerve is the primary nerve of the parasympathetic autonomic nervous system. We can most directly stimulate the vagus nerve and parasympathetic activity with electrical auricular vagus nerve stimulation. The homeostatic effect is amplified by connecting the 3 parasympathetic-dominant regions of the body to each other with low frequency microcurrent, 1-5 Hz (I like 1 Hz because it is closest to a typical heartbeat) – the auricular branch of the vagus nerve in the ear, this is the most direct, the sacral plexus, S2-S4, and the suboccipital / C2 spinous process periosteum.
For more information on vagus nerve stimulation, check this out:
Electrical Dry Needling for Auricular Vagus Nerve Stimulation to Reduce Sympathetic Autonomic Nervous System Hyperactivity & Regulate the ANS Toward Homeostasis:
What is Pistoning?
The pistoning technique involves a sewing-machine, or jack-hammer-like motion of the needle going in and out of tissue. The needle is not fully removed from tissue following initial insertion, but is poked in and out of the tissue at varying angles, with the goal of puncturing numerous locations of trigger points (hypercontracted groups of sarcomeres), or other pathologic tissue. Once the poking is done, the needle is removed. Get your mind out of the gutter people! There is also no twisting of the needle and there is no electrical stimulation applied. This is how the majority of practitioners dry needle in the United States. This approach to needling completely disregards the neurophysiologic state of our patient’s mind and body. Sympathetic autonomic nervous system hyperactivity.
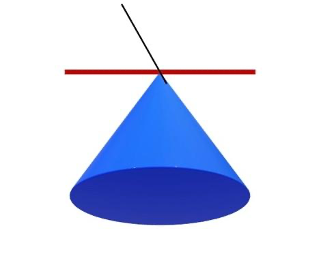
For this discussion, let’s define pistoning as 10 advances of a 0.2 mm diameter needle into an area of tissue in a cone shape. Following the 10 advances, the needle is removed. This is common practice in Pistoning-Land. In the image below, think of the red line as the skin, the black line is the needle, and the blue cone is the tissue the needle is inserted into. Advancing a 0.2 mm diameter needle 10 times allows you to treat a circle of tissue with a 2 mm diameter (0.2 mm x 10 = 2 mm). A circle with a 2 mm diameter has an area of 3.14 mm2. So, the bottom of the cone is about 3.14 mm2 with a diameter of 2 mm.
Note: The math in this article is as accurate as I could get without more advanced equipment. I am sure this is off a bit, but I think it conveys the general state of matters. I would love any thoughts on this from fellow needlers or if anyone has more data on this.
Should I Piston?
The short answer? No, you should not, in general. Now, there are instances when pistoning is useful. However, it should only be utilized in specific circumstances, with specific patients. There are numerous reasons for this. You should never piston over the lung field, bladder, or anything else you do not want to hit. In reality, you can likely hit just about anything in the body 1 time with a solid, 0.2 mm thick piece of surgical steel and never cause any noticeable damage. You would probably never know anything happened. Remember, normal, hollow needles are typically somewhere between 1-2 mm, and those are stuck into vessels, organs, etc., all the time, on purpose, without a problem. Hitting something more than once in a small area is when you run an increased risk of significant damage. Not pistoning decreases risk, as far as vasovagal response and tissue damage goes, and improves treatment efficacy via improved autonomic nervous system homeostasis. Remember, MD’s take chunks out of organs to biopsy them in the lab. The intestines and heart can be sutured, the lungs and bladder can be drained. All this is done with needles or cutting instruments exponentially larger than the tiny, solid, 0.2 mm, or so, thick needles we utilize. Aside from increasing safety and efficacy, not pistoning is exponentially more comfortable for the patient, part of the reason it increases efficacy. This is important.
Pistoning, in general, makes negative neurophysiologic sense. One goal of dry needling should be removing as much pathologic tissue throughout the body as possible, with the express intent of depressing sympathetics, elevating parasympathetics, and guiding the autonomic nervous system toward homeostasis, allowing the body to heal the mind and the mind to heal the body. This involves treating the body as an intricately interconnected complex system.
If a pistoner inserts a single needle 10 times into the same small area of tissue, you are stimulating the sympathetics 10 times. If you use 2 needles, that is 20 times the sympathetics are stimulated in the process of treating an overall area of (3.14 mm2 x 2) 6.28 mm2 of tissue.
Now, take a peek at the ultrasound image below from Helen Langevin, MD, a world-renowned researcher on the effects of acupuncture on soft tissue. The black dot in the left picture is a needle placed in tissue without rotating it. I look at this as the needle treating only the tiny bit of tissue it is through, the black dot. The picture on the right is after the needle has been rotated until it won’t turn anymore. In this picture, the entire square, and more, is being treated. I copied the scale bar and imposed it over the right picture in the blue lines. Each of the blue lines is 1 mm. There are 7 lines there. So, the area of each square image is about 7 mm x 7 mm = 49 mm2.
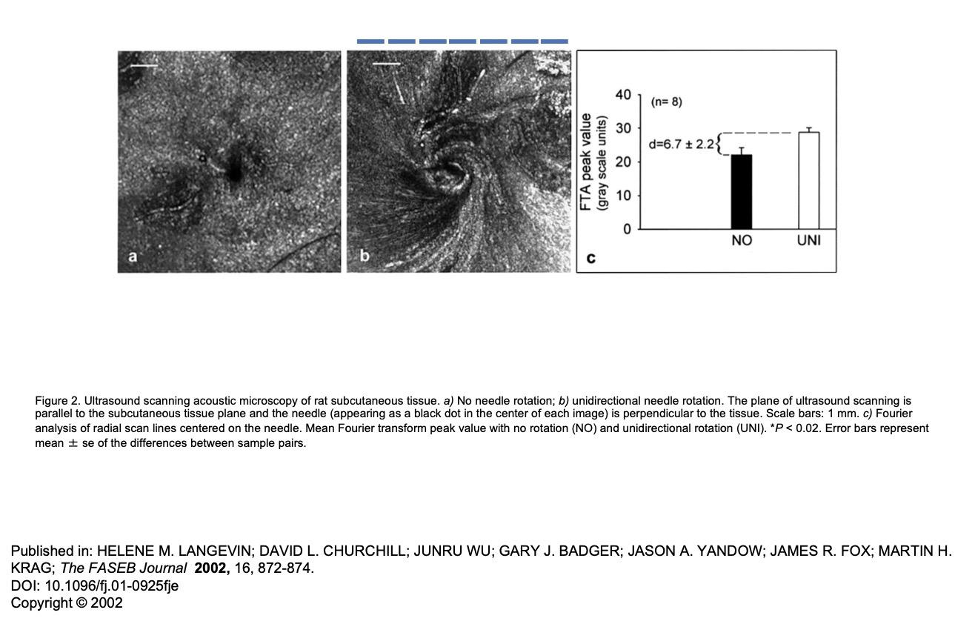
By inserting 2 needles, one time each, and rotating them until tight (49 mm x 2), you treat about 98 mm2 of tissue with 2 needle advances, or two stimuli to the sympathetics. Compare this to pistoning, where with 2 needles, advancing each 10 times into tissue, without needle rotation, you elicit 20 stimuli to the sympathetics, while only treating 6.28 mm2 of tissue. So, with pistoning, you are eliciting 10 times the sympathetic autonomic stimulation and treating about 15 times less tissue area (98 mm2 / 6.28 mm2 = 15) . Which one seems better to you?
Furthermore, if you advance each needle once and twist it, rather than 10 times each without twisting, you can use 20 needles to treat 980 mm2 of tissue (156 times more tissue) and stimulate the sympathetics the same amount as if you pistoned with only 2 needles, covering only 6.28 mm2 of tissue (980 mm2 / 6.28 mm2 = 156).
Pistoning Technique
2 needles x 10 needle advances per needle = 20 sympathetic stimuli covering 3.14 x 2 mm2) = 6.28 mm2 of tissue.
Intricate Art single Advancement Technique
20 needles x 1 needle advance per needle = 20 sympathetic stimuli covering 20 x 49 mm2 = 980 mm2 of tissue.
980 mm2 divided by 6.28 mm2 = 156. That means, with 1 advancement into tissue per needle, you can treat 156 times the area of tissue with the same amount of sympathetic stimulation as compared to pistoning. Or, you can treat the same amount of tissue area with our technique as with pistoning, while stimulating the sympathetics 16 times less (49 mm2 / 3.14 mm2 = 15.6). Again, the goal is to treat as much pathologic tissue with as little sympathetic stimulation as possible. The end-goal is sympathetic depression, parasympathetic elevation, and autonomic homeostasis, so which technique is more logical? The last thing physical therapy patients need is more sympathetic autonomic hyperactivity. They are already suffering, at least in part, specifically because they are living with chronic sympathetic autonomic nervous system hyperactivity.
The only time I will utilize pistoning is if I get a twitch out of the muscle and I want to see if I can elicit more twitches. When you hit a knot with a needle, a lot of the time you elicit a twitch, or muscle contraction. This is secondary to a bunch of sarcomeres unlocking from each other. This is the fastest way to dissolve trigger points. It can really hurt, which is not a negative thing, however, it will scare a lot of people away from future needling treatment, depending on their personality. I do not piston the first few treatments when introducing a patient to needling, and you should never do pistoning if the patient is hypersensitive or prone to vasovagal response, as this significantly amplifies pain and sympathetic stimulation. Again, our patients live with chronic sympathetic hyperactivity. Everything in our power should be done to depress sympathetics and elevate parasympathetics, leading the autonomic nervous system toward homeostasis.
Thanks for reading. Let me know if anyone has any questions about anything. Talk to you soon.
Jason
DISCLAIMER: The content on the blog for Intricate Art Spine & Body Solutions, LLC is for educational and informational purposes only, and is not intended as medical advice. The information contained in this blog should not be used to diagnose, treat or prevent any disease or health illness. Any reliance you place on such information is therefore strictly at your own risk. Please consult with your physician or other qualified healthcare professional before acting on any information presented here.
References
- Butts, R., Dunning, J. and Serafino, C., 2021. Dry needling strategies for musculoskeletal conditions: Do the number of needles and needle retention time matter? A narrative literature review. Journal of Bodywork and Movement Therapies, 26, pp.353-363.
- Kearns, G.A., Brismée, J.M., Riley, S.P., Wang-Price, S., Denninger, T. and Vugrin, M., 2022. Lack of standardization in dry needling dosage and adverse event documentation limits outcome and safety reports: a scoping review of randomized clinical trials. Journal of Manual & Manipulative Therapy, pp.1-12.
- Padanilam, S.J., Dayton, S.R., Jarema, R., Boctor, M.J. and Tjong, V.K., 2021. Dry Needling for the Treatment of Musculoskeletal Ailments With Trigger Points. Video Journal of Sports Medicine, 1(5), p.26350254211023776.
- Butt, M.F., Albusoda, A., Farmer, A.D. and Aziz, Q., 2020. The anatomical basis for transcutaneous auricular vagus nerve stimulation. Journal of anatomy, 236(4), pp.588-611.
- Garner, B.K., Hopkinson, S.G., Ketz, A.K., Landis, C.A. and Trego, L.L., 2018. Auricular acupuncture for chronic pain and insomnia: a randomized clinical trial. Medical acupuncture, 30(5), pp.262-272.
- Jaić, K.K., Turković, T.M., Pešić, M., Djaković, I., Košec, V. and Košec, A., 2019. Auricular acupuncture as effective pain relief after episiotomy: a randomized controlled pilot study. Archives of gynecology and obstetrics, 300(5), pp.1295-1301
- Johnson, R.L. and Wilson, C.G., 2018. A review of vagus nerve stimulation as a therapeutic intervention. Journal of inflammation research, 11, p.203.
- Kang, H.R., Lee, Y.S., Kim, H.R., Kim, E.J., Kim, K.H., Kim, K.S., Jung, C.Y. and Lee, J.K., 2017. A clinical study of electroacupuncture and auricular acupuncture for abdominal pain relief in patients with pancreatitis: A pilot study. Korean Journal of Acupuncture, 34(1), pp.47-55.
- Moura, C.D.C., Chaves, E.D.C.L., Cardoso, A.C.L.R., Nogueira, D.A., Azevedo, C. and Chianca, T.C.M., 2019. Auricular acupuncture for chronic back pain in adults: a systematic review and metanalysis. Revista da Escola de Enfermagem da USP, 53.