Dry Needling & Joint Manipulation to Treat & Resolve Hiccups
Dr. Andrew Huberman, who I love and highly recommend, recently spoke about hiccups and how to resolve them, along with some awesome information on how to regulate the autonomic nervous system via sympathetic autonomic depression with certain breathing techniques.
Video: Dr. Huberman on Hiccups
Dr. Huberman mentioned the best way to resolve hiccups is to reduce spasms of the phrenic nerves and the diaphragm, which the phrenic nerves innervate. To accomplish this, Dr. Huberman recommends taking 3 consecutive inhales through your nose, without exhaling, maximally inflating the lungs, then hold the last inhale for about 20 seconds before exhaling. What this does is it forces your diaphragm to contract 3 consecutive times, secondary to 3 consecutive phrenic nerve action potentials, without relaxing, since inhaling typically involves contraction of the diaphragm. This tires out the phrenic nerve and the diaphragm, which causes temporary relaxation and reduction of diaphragmatic spasms, resulting in resolution of hiccups.
However, this technique works via amplification of the underlying mechanism causing hiccups. Sympathetic autonomic nervous system hyperactivity. Forcing excessive contraction of the diaphragm elevates sympathetics. Excessive, conscious contraction of muscle is a sympathetic-dominant neurophysiologic process. Like hiccups. Again, and this is not super easy to grasp, this breathing technique works by turning up the part of the nervous system that is already turned up too high, the sympathetics, but the extra stimulation, acutely, in the immediate short-term, exhausts the innervated structures, the diaphragm in this case, leading to temporary relaxation.
This is the same reasoning practitioners typically use when they apply electrical stimulation patches, or electrical stimulation through needles. Most people that use electrical stimulation are taught to make the stimulus “strong but comfortable.” This is a mistake, as it amplifies sympathetics, which are already in a state of hyperactivity. I’m not saying it doesn’t work, it does. It leads to short term paradoxical results, because repetitive muscle contraction tires out the muscle and creates a temporary state of inhibition. Dr. Huberman is correct that this is a great method to resolve hiccups. It is probably the best quick fix, unless you always have needles with you, which is not weird or anything... However, it is not the best overall fix. Thoughtful dry needling combined with joint manipulation is the best way to treat and resolve hiccups, and leads to more permanent results. This is because, if performed correctly, it addresses the underlying cause of sympathetic hyperactivity by removing sympathetic stress throughout the body and directly targeting the opposing part of the autonomic nervous system, the parasympathetic autonomic nervous system. This leads to rapid, significant, lasting improvements with hiccups, autonomic nervous system homeostasis, and overall health.
Hiccups, like most things in medicine, are not completely understood and can be associated with a multitude of other symptoms. However, like the overwhelming majority of medical impairments, hiccups cause, and are a result of, sympathetic autonomic nervous system hyperactivity, typically. Overall, sympathetic hyperactivity lowers action potential threshold and makes it easier for spontaneous electrical activity and muscle firing to occur. Exactly what happens in hiccups. Muscle spasm is a hallmark sign of chronic sympathetic hyperactivity. Hiccups are from a muscle spasm in your diaphragm.
Chronic Sympathetic Hyperactivity Leads to, and is a Cause of:
- Excessive norepinephrine
- Excessive intracellular calcium
- Excessive acetylcholine
- Decreased acetylcholine esterase
- Increased receptivity of muscle epimysium to acetylcholine
- Chronic muscle cell depolarization, making the tissue more negative, making spontaneous firing more likely
- Increased vasoconstriction
- Increased tissue hypoxia, including nerve hypoxia
- Increased pain
- Increased proinflammatory markers, like IL-1, IL-6, & TNF-a
- Increased cortisol
- Increased anxiety
- Increased muscle spasms
- Decreased muscle length
- Decreased GABA
- Increased glutamate
All of this nonsense drives further sympathetic hyperactivity and becomes a nasty, detrimental feedback loop. When this feedback loop involves the phrenic nerves and diaphragm, it causes hiccups. One of the underlying strategies I employ when teaching and treating patients is to always maximize the body and mind’s awesome, innate abilities to heal and self-regulate themselves and each other. This typically involves depressing the sympathetics and stimulating the parasympathetics with the goal of inducing autonomic nervous system homeostasis. This will help with all aspects of mental and physical health, including hiccups.
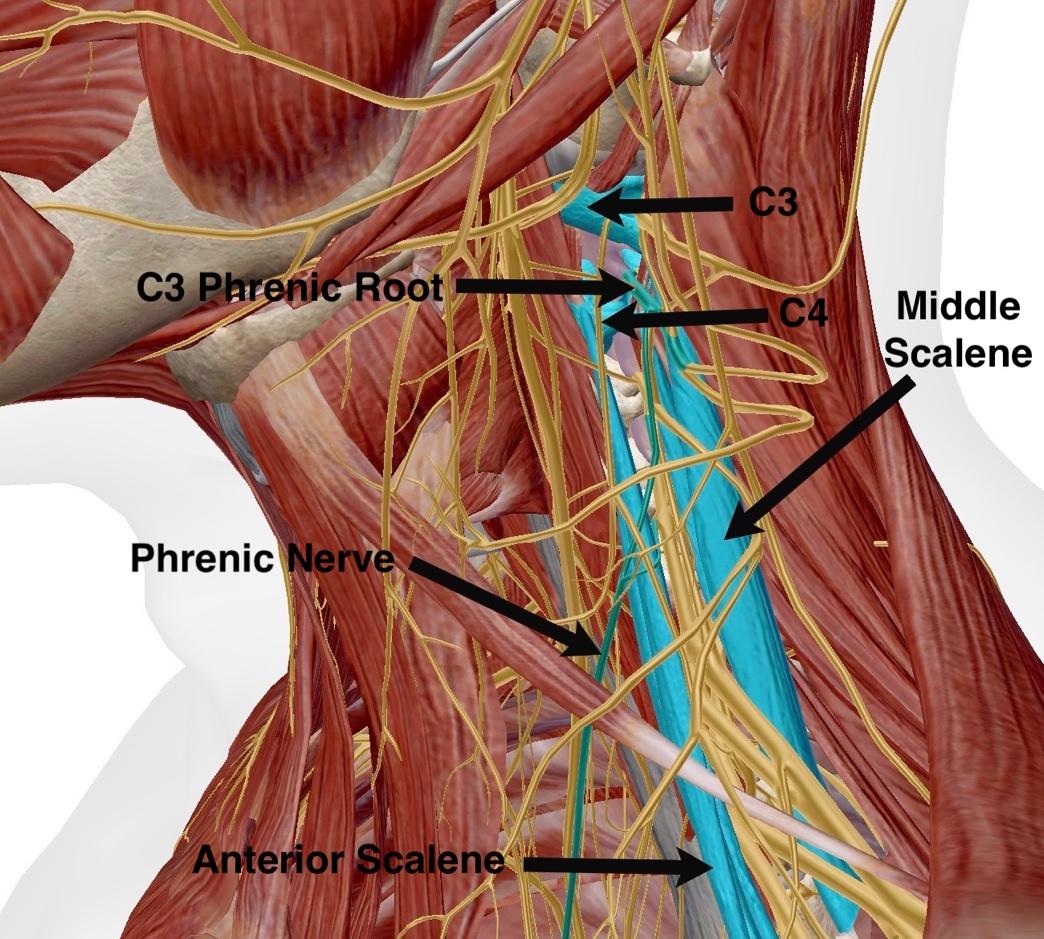
The Phrenic Nerve, Anterior Scalene, & Middle Scalene
The phrenic nerve originates from the C3, C4, and C5 spinal nerve roots. “C3, 4, and 5 keep you alive” is a common saying, referring to the fact that the diaphragm, the primary breathing muscle, is innervated by the phrenic nerve. Notice the orientation of the anterior and middle scalene muscles in the picture above. They are the two closest muscles to the phrenic nerve roots. The anterior scalene originates on the anterior aspect of C3-C6 transverse processes. The middle scalene originates on the posterior aspect of C2-C7 transverse processes. Both the anterior and middle scalenes attach to the top of the first rib. I think about the anterior and middle scalenes as kinda making a sandwich out of the phrenic nerve roots and the transverse processes of C3-C5. The issue here is, if the scalenes get grumpy, and let me tell you, they get cranky real easy, the whiny wimps, the phrenic nerve roots get squished. They get squished when the two scalenes contract, thickening, and pushing in on the nerve roots, as well as from branches of C3-C5 nerve roots getting crushed as they pass through the scalene muscles themselves. Squished nerve roots are no bueno. Squished nerve roots lead to hypoxic nerves, which leads to spontaneous electrical firing and muscle spasms. Spontaneous electrical firing of the phrenic nerve causes muscle spasms in the diaphragm, which causes hiccups.
Another contributing factor to hiccups is the fact that the scalenes attach to the first rib. If they get tight, not only do they compress the phrenic nerve in multiple ways, they pull the first rib upward and out of place. Cephalic first rib displacement is a leading cause of thoracic outlet syndrome (TOS) and contributes to hiccup production. When the first rib gets displaced, it places abnormal stresses on the stellate ganglion, which sits just in front of the first rib head. The stellate ganglion is often considered the superior portion of the sympathetic chain, part of the sympathetic autonomic nervous system. Remember, the sympathetic chain runs from the stellate ganglion at C7/T1 down to the lumbar spine on the anterolateral aspect of the vertebral bodies, according to most books. So, the anterior and middle scalenes have pretty direct access to push on the phrenic and pull on the sympathetic chain, both of which can cause hiccups, along with a multitude of other impairments. Chronic abnormal stresses on the sympathetic chain can cause just about any impairment you can think of.

C1/C2 & Hiccups
So, we have spoken about muscles and nerves so far in relation to sympathetic hyperactivity and hiccups. Joints are super important too. Especially C1/C2. C1/C2 is the most mobile segment in our spine and C1 has the most individual movement out of all 33 vertebrae. C1/2 accounts for about 50% of our total cervical rotation. If you have 90 degrees of cervical rotation to the left, 45 of those degrees are coming from C1/C2. The other 45 degrees is split between the other cervical segments, with no other segment producing more than 15 degrees of rotation. Remember from above, the middle scalene attaches directly to the C2 transverse process. Any muscle with a direct C2 attachment, when pathologic, has a good chance of causing significant C1/C2 deviation, including the middle scalene. Since C1/C2 moves so much, this also makes it the easiest spinal segment for our body to use to compensate for deviation elsewhere in the spine.

Another thing about the C1/C2 segment is the trigeminocervical nucleus, part of the trigeminocervical complex. The trigeminocervical nucleus sits in the dorsal horn of the spinal cord at about C2. If C1/C2 becomes deviated, which it is in most people, not only does it place abnormal tension through the scalenes, which directly push on the phrenic nerve and strain the stellate ganglion via first rib displacement, the trigeminocervical nucleus begins to receive pathologic afferent signals and short circuits. This leads to further sympathetic hyperactivity, making hiccups, and overall mental and physical health, worse.
Other Muscles to Think About When Treating Hiccups
Another three important muscles to target when treating hiccups are the multifidus, psoas major, and the quadratus lumborum. The multifidus is my favorite muscle in the body to treat and is one of the most important muscles in the body to have fully functional. The psoas major is my second favorite muscle. Unfortunately, the multifidus and psoas major are complete disaster areas in most people. They are the deepest, major skeletal muscles in our bodies, are two of our most important core and spinal stabilizers, and are the closest muscles to the sympathetic chain. This is key. The origin and insertion of the multifidus is often considered to be C2 spinous process and S2 periosteum, respectively. The origin of the psoas major is the anterior aspect of the lumbar transverse processes and the anterolateral aspects of the lumbar vertebral bodies, and the insertion is on the lesser trochanter of the femur. We will get to the QL’s in a sec, let's stick with the multifidus and psoas for the moment.
The multifidus covers the majority of the spine, and in instances of chronic sympathetic hyperactivity, becomes infiltrated with adipose tissue (fat). There is no definitive explanation as to why this happens. There are likely lots of reasons, however, one common thread between all the reasons it can happen is apparent. Chronic Sympathetic autonomic hyperactivity. The same reason we get hiccups! The sympathetic chain sits just on the anterolateral side of the vertebral bodies and the multifidus lives in the posterolateral aspect of the spine. The psoas major is the closest muscle to the sympathetic chain on the anterior side of the lumbar spine. Sympathetic chain, psoas, and multifidus pathology are intertwined. Muscle pathology can aggravate the sympathetic chain and sympathetic chain pathology can aggravate the muscles. Whatever happens first, after a certain time, the presence of one drives the other in a destructive, detrimental feedback loop, with the end result being more sympathetic hyperactivity. With enough sympathetic hyperactivity, the tendrils of the sympathetic chain that pass through the multifidus and psoas major elicit elevation of sympathetic tone. This increases muscle tonicity, increases spinal compression, decreases blood flow, increases hypoxia, increases pain, and leads to further elevation of the sympathetics, along with muscle dysfunction.
The multifidus must be functional to have optimal stabilization of the C1/C2 segment, since it is one of the muscles attaching to C2, including the middle scalene. If the multifidus is pathologic, not only does it lead to abnormal stresses on the sympathetic chain and sympathetic nervous system, it leads to C1/C2 deviation and subsequent aggravation of the trigeminocervical nucleus in the spinal cord at C2. This leads to even more dysregulation of the autonomic nervous system and a plethora of other potential impairments, including hiccups.
Quadratus Lumborum
A Muscle I like to think of in relation to the scalenes is the quadratus lumborum (QL). The scalenes attach the first rib to the cervical transverse processes. The QL attaches the 12th rib to lumbar transverse processes and the pelvis (iliac crest). If the scalenes get tight they pull the first rib and the ribcage up. If the QL’s get tight, they pull the 12th rib and ribcage down. If the QL’s and scalenes are both tight, which they often are, this makes it much easier for the scalenes to displace the first rib upward. Again, this leads to abnormal stresses, strains, and inflammation around the thoracic outlet the phrenic nerve root exits at C3-C5, which can lead to hiccups.
Quadratus Lumborum (QL)

Summary
So, use Dr. Huberman’s technique to immediately resolve hiccups, and use dry needling and joint manipulation to permanently resolve hiccups, along with a multitude of other impairments. You can totally use dry needling and manipulation to immediately resolve hiccups, however, this is not typically feasible. Remember, resolving hiccups includes the same general thought process that should be included in all dry needling and manipulative treatment. Think about what muscles, joints, and nerves may specifically be causing the problem, while concomitantly thinking about maximizing autonomic nervous system homeostasis to allow the mind and the body to utilize their awesome, innate healing powers. This includes targeting of specific nerves and muscles, along with removing as much pathologic tissue throughout the body, while at the same time targeting the parasympathetic portion of the autonomic nervous system, with the end goal being autonomic nervous system homeostasis and resolution of hiccups.
DISCLAIMER: The content on the blog for Intricate Art Spine & Body Solutions, LLC is for educational and informational purposes only, and is not intended as medical advice. The information contained in this blog should not be used to diagnose, treat or prevent any disease or health illness. Any reliance you place on such information is therefore strictly at your own risk. Please consult with your physician or other qualified healthcare professional before acting on any information presented here.
References
- Verlinden, T.J.M., van Dijk, P., Herrler, A. et al. The human phrenic nerve serves as a morphological conduit for autonomic nerves and innervates the caval body of the diaphragm. Sci Rep 8, 11697 (2018). https://doi.org/10.1038/s41598-018-30145-x.
- /dry-needling-idiopathic/
- /the-intricate-interconnectivity-of-the-jaw/
- /dry-needling-for-erectile-dysfunction/