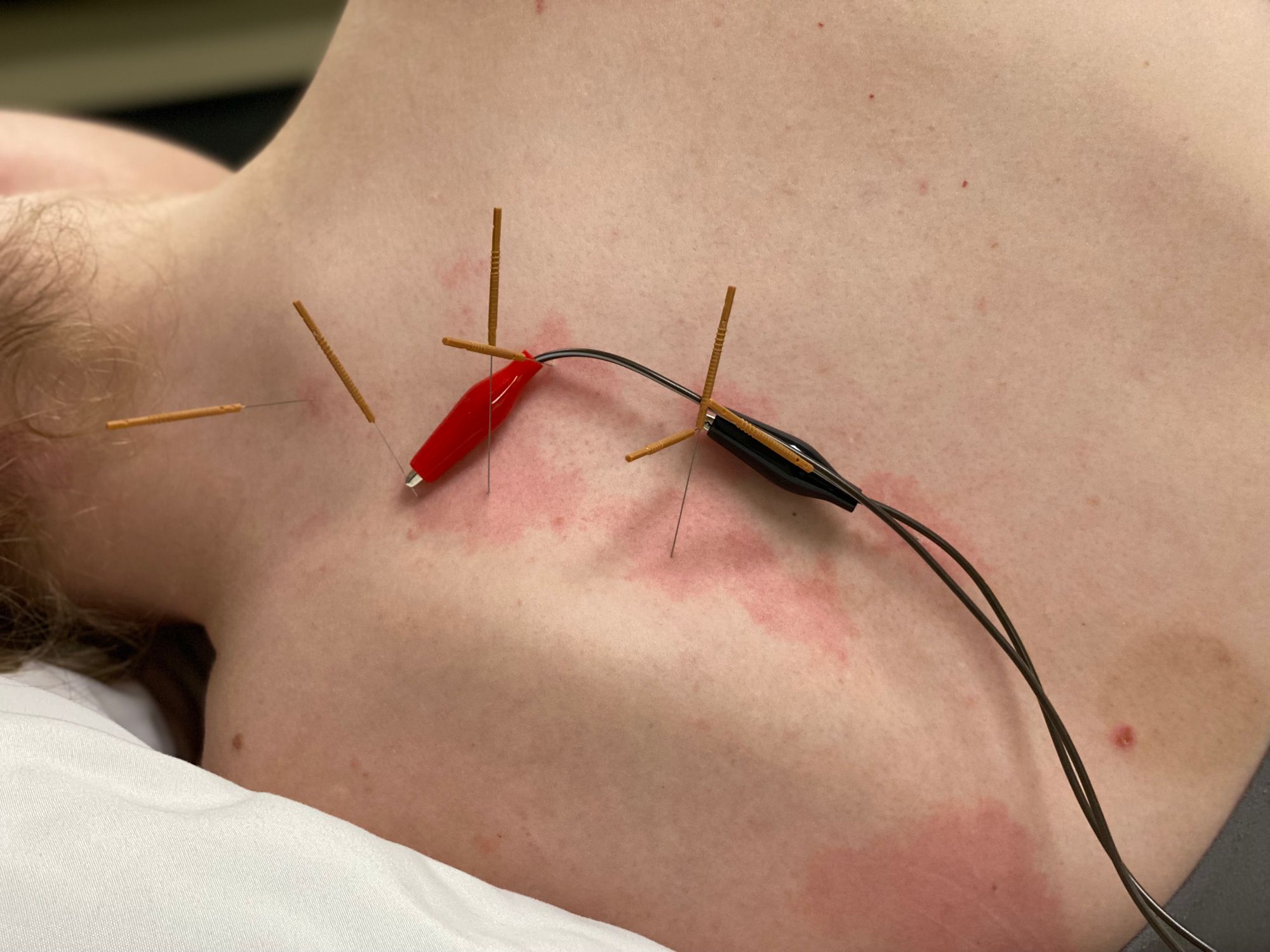
How Does Dry Needling Work? Part 1
A lot of students have asked me to recap how I explain the mechanisms of action, that we somewhat understand, regarding how dry needling works. This is part 1 of what I typically say to other medical professionals:
So, DN works on 2 primary levels. Mechanical and neurologic, although I believe the mechanical changes are primarily driven by the nervous systems changes induced by needling. On a mechanical level, there are a bunch of things that need to happen for a muscle to contract, but there are a few primary things that need to occur. Let’s think about this in terms of a sarcomere and the actin and myosin cross-bridge formation.
Normal Skeletal Muscle Contraction
The primary things that need to happen for an actin-myosin cross-bridge to form are: Acetylcholine, a neurotransmitter, needs to cross the synaptic cleft to the post-synaptic terminal, which signals the Sodium-Potassium pump to depolarize the cell. Troponin needs to be present inside the sarcomere and calcium needs to be released from the sarcoplasmic reticulum, which is already intracellular. Troponin and calcium bind together, move tropomyosin out of the way, and form the cross-bridge site for the actin-myosin attachment.
Normal Skeletal Muscle Relaxation
The primary things that need to happen to disconnect the actin-myosin cross-bridge are: Tropomyosin enters the cell and breaks the calcium-troponin bond. Calcium gets reabsorbed into the sarcoplasmic reticulum. Acetylcholine esterase needs to be present in sufficient concentration to gobble up all the acetylcholine and the sarcomere becomes repolarized.
Note: Remember, normal resting muscle cell potential for skeletal muscle is about -35 millivolts, or so. An action potential typically occurs at -70 millivolts, or so. Also remember the vast majority of PT patients present with sympathetic hyperactivity of both the ANS and CNS. With hyperactive sympathetics, the resting potential of the sarcomere is more negative, maybe at -45 millivolts, and the action potential is less negative, maybe around -60 millivolts. In this instance, the electrical potential of the cell needs to change far less to stimulate an action potential. This is one of the reasons that sympathetically hyperactive sarcomeres produce spontaneous electrical activity.
Related: Looking for a video version of this blog? Click here to watch.
Abnormal Skeletal Muscle Contraction & Relaxation Secondary to Sympathetic Hyperactivity
With hyperactive sympathetics, as mentioned above, the action potential threshold is diminished. Hyperactive sympathetics also lead to skeletal muscle vasoconstriction and trigger points, which are just groups of hypercontracted sarcomeres. This leads to hypoxic tissues with excessive CO2 concentrations. excessive CO2 concentration makes the cell more acidic, making muscles more likely to spontaneously fire and hindering enzyme function.
Hyperactive sympathetics lead to excessive acetylcholine production / release, diminished acetylcholine esterase production / release, along with excessive intracellular calcium concentration. These factors make it next-to-impossible for the actin-myosin cross-bridge to disconnect. A negative feedback loop ensues where the muscles hurt, they contract more, become more hypoxic, even more detrimental concentrations of chemicals arise, many of which are pain amplifiers, the muscle cannot relax, it hurts more, and so on..
Another thing that happens with chronically hyperactive sympathetics is, rather than just the post synaptic cleft being receptive to acetylcholine, the entire epimysium (muscle lining) becomes receptive to acetylcholine. With excessive concentrations of acetylcholine and the entire epimysium becoming receptive to it, a slow, chemical shortening of muscles begins. This is not active, spontaneous electrical contraction, it is a chemical contraction, which may not show up on an EMG.
Hyperactive sympathetics also dysregulate the hypothalamic-pituitary-adrenal (HPA) axis and the gut-brain-axis (enteric nervous system + brain), both part of the ANS. If these axes are dysregulated, all of our hormones, peptides, neurotransmitters, immune systems, etc., become dysregulated and malfunction. This can lead to just about any medical impairment.
Dry needling is, without question, the most powerful tool PT’s have at their disposal to quickly and effectively regulate the CNS and ANS toward homeostasis, which, in turn, regulates our muscle health. Without CNS / ANS homeostasis, nothing in our body works properly. Remember, the overall effect of needling, almost regardless of how it is performed, results in CNS / ANS sympathetic depression below baseline and parasympathetic elevation above baseline. This works out well for us, since the significant majority of PT patients present with sympathetic hyperactivity. This works especially well if you specifically target the PANS with needles, along with whatever else you are needling. This decreases the amplitude and duration of the initial sympathetic spike following needle insertion, which typically lasts about 15 minutes, according to numerous heart rate variability and microneurography (gold standard ANS test) studies. If PANS-specific needles are implemented, the body and mind are allowed more treatment time with the body in parasympathetic dominance, making treatment more effective, lasting, and comfortable for your patients.
Now, these are a few of the things we think we have a decent grasp on. However, to remind you, we don’t even know for sure how a muscle contracts! It is still called the sliding filament theory for a reason. It is still a theory. I always think about this; if it was possible to quantitatively assess all the medical knowledge available out there in the ether, I bet we know less than 5% of the whole. If you really think about it, we have very few 100% fixes for any medical condition. Most of the treatments we have today are just Band-Aids that mask the symptoms of the underlying problem. They don’t actually address the cause of the problem, limiting their efficacy and maximizing side-effects. This, in part, is because the pharmaceutical companies would rather not have any 100% cures for diseases. It is much more profitable to keep people partially sick for life. That way, you give them medicines that only mask symptoms, and if the medicine causes side effects, you get more medicine to counter the side effects of the original medicine you were taking. It’s disgusting. Unfortunately, the one thing that rarely gets addressed, an important aspect of medicine, is treating everyone as an individual and addressing the root cause of the problem, along with the symptoms. Not just the symptoms.
Dry needling is one of the few treatments in Medical-Land that addresses both the cause of the problem and the symptoms, for just about any impairment out there. Again, I don’t know of any medical impairment that is not helped by improved CNS / ANS homeostasis, and needling is the most powerful tool PT’s have at their disposal to regulate the neuromusculoskeletal system.
Let me know if anyone has any questions about anything. Talk to you soon.
Jason
DISCLAIMER: The content on the blog for Intricate Art Spine & Body Solutions, LLC is for educational and informational purposes only, and is not intended as medical advice. The information contained in this blog should not be used to diagnose, treat or prevent any disease or health illness. Any reliance you place on such information is therefore strictly at your own risk. Please consult with your physician or other qualified healthcare professional before acting on any information presented here.
References
Muscle Contraction
- Stojanovic, B., Svicevic, M., Kaplarevic-Malisic, A., Gilbert, R.J. and Mijailovich, S.M., 2020. Multi-scale striated muscle contraction model linking sarcomere length-dependent cross-bridge kinetics to macroscopic deformation. Journal of Computational Science, 39, p.101062.
- Senneff, S. and Lowery, M.M., 2021. Effects of extracellular potassium on calcium handling and force generation in a model of excitation-contraction coupling in skeletal muscle. Journal of Theoretical Biology, 519, p.110656.
- Carter, S. and Solomon, T.P., 2019. In vitro experimental models for examining the skeletal muscle cell biology of exercise: the possibilities, challenges and future developments. Pflügers Archiv-European Journal of Physiology, 471(3), pp.413-429.
- Michailowsky, V., Li, H., Mittra, B., Iyer, S.R., Mazála, D.A.G., Corrotte, M., Wang, Y., Chin, E.R., Lovering, R.M. and Andrews, N.W., 2019. Defects in sarcolemma repair and skeletal muscle function after injury in a mouse model of Niemann-Pick type A/B disease. Skeletal muscle, 9(1), pp.1-15.
- Stern, M.D., Pizarro, G. and Ríos, E., 1997. Local control model of excitation–contraction coupling in skeletal muscle. The Journal of general physiology, 110(4), pp.415-440.
- Rebbeck, R.T., Karunasekara, Y., Board, P.G., Beard, N.A., Casarotto, M.G. and Dulhunty, A.F., 2014. Skeletal muscle excitation–contraction coupling: who are the dancing partners?. The international journal of biochemistry & cell biology, 48, pp.28-38.
- Gong, G., Liu, X. and Wang, W., 2014. Regulation of metabolism in individual mitochondria during excitation–contraction coupling. Journal of molecular and cellular cardiology, 76, pp.235-246.
- Qaisar, R., Bhaskaran, S., Premkumar, P., Ranjit, R., Natarajan, K.S., Ahn, B., Riddle, K., Claflin, D.R., Richardson, A., Brooks, S.V. and Van Remmen, H., 2018. Oxidative stress‐induced dysregulation of excitation–contraction coupling contributes to muscle weakness. Journal of cachexia, sarcopenia and muscle, 9(5), pp.1003-1017.
- Hernández-Ochoa, E.O. and Schneider, M.F., 2018. Voltage sensing mechanism in skeletal muscle excitation-contraction coupling: coming of age or midlife crisis?. Skeletal muscle, 8(1), pp.1-20.
- Squire, J.M., 2016. Muscle contraction: Sliding filament history, sarcomere dynamics and the two Huxleys. Global cardiology science & practice, 2016(2).
- Rassier, D.E., 2017. Sarcomere mechanics in striated muscles: from molecules to sarcomeres to cells. American Journal of Physiology-Cell Physiology, 313(2), pp.C134-C145.
- Powers, J.D., Malingen, S.A., Regnier, M. and Daniel, T.L., 2021. The sliding filament theory since Andrew Huxley: multiscale and multidisciplinary muscle research. Annual review of biophysics, 50, pp.373-400.
- Nishikawa, K., Dutta, S., DuVall, M., Nelson, B., Gage, M.J. and Monroy, J.A., 2020. Calcium-dependent titin–thin filament interactions in muscle: observations and theory. Journal of Muscle Research and Cell Motility, 41(1), pp.125-139.
Vagus Nerve Stimulation
- Sprouse-Blum, A.S., Smith, G., Sugai, D. and Parsa, F.D., 2010. Understanding endorphins and their importance in pain management. Hawaii medical journal, 69(3), p.70.
- Usichenko, T.I., Dinse, M., Hermsen, M., Witstruck, T., Pavlovic, D. and Lehmann, C., 2005. Auricular acupuncture for pain relief after total hip arthroplasty–a randomized controlled study. Pain, 114(3), pp.320-327.
- Usichenko, T.I., Kuchling, S., Witstruck, T., Pavlovic, D., Zach, M., Hofer, A., Merk, H., Lehmann, C. and Wendt, M., 2007. Auricular acupuncture for pain relief after ambulatory knee surgery: a randomized trial. Cmaj, 176(2), pp.179-183.
- Jaić, K.K., Turković, T.M., Pešić, M., Djaković, I., Košec, V. and Košec, A., 2019. Auricular acupuncture as effective pain relief after episiotomy: a randomized controlled pilot study. Archives of gynecology and obstetrics, 300(5), pp.1295-1301
- Taylor, S.L., Giannitrapani, K.F., Ackland, P.E., Thomas, E.R., Federman, D.G., Holliday, J.R., Olson, J., Kligler, B. and Zeliadt, S.B., 2021. The Implementation and Effectiveness of Battlefield Auricular Acupuncture for Pain. Pain Medicine.
- Shah, A.N., Moore, C.B. and Brigger, M.T., 2020. Auricular acupuncture for adult tonsillectomy. The Laryngoscope, 130(8), pp.1907-1912.
- Garner, B.K., Hopkinson, S.G., Ketz, A.K., Landis, C.A. and Trego, L.L., 2018. Auricular acupuncture for chronic pain and insomnia: a randomized clinical trial. Medical acupuncture, 30(5), pp.262-272.
- Kang, H.R., Lee, Y.S., Kim, H.R., Kim, E.J., Kim, K.H., Kim, K.S., Jung, C.Y. and Lee, J.K., 2017. A clinical study of electroacupuncture and auricular acupuncture for abdominal pain relief in patients with pancreatitis: A pilot study. Korean Journal of Acupuncture, 34(1), pp.47-55.
- Moura, C.D.C., Chaves, E.D.C.L., Cardoso, A.C.L.R., Nogueira, D.A., Azevedo, C. and Chianca, T.C.M., 2019. Auricular acupuncture for chronic back pain in adults: a systematic review and metanalysis. Revista da Escola de Enfermagem da USP, 53.
- Tsai, S.L., Fox, L.M., Murakami, M. and Tsung, J.W., 2016. Auricular acupuncture in emergency department treatment of acute pain. Annals of emergency medicine, 68(5), pp.583-585.
- Yeh, C.H., Chiang, Y.C., Hoffman, S.L., Liang, Z., Klem, M.L., Tam, W.W., Chien, L.C. and Suen, L.K.P., 2014. Efficacy of auricular therapy for pain management: a systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine, 2014.
- Sator-Katzenschlager, S.M., Szeles, J.C., Scharbert, G., Michalek-Sauberer, A., Kober, A., Heinze, G. and Kozek-Langenecker, S.A., 2003. Electrical stimulation of auricular acupuncture points is more effective than conventional manual auricular acupuncture in chronic cervical pain: a pilot study. Anesthesia & Analgesia, 97(5), pp.1469-1473.
- Usichenko, T.I., Lehmann, C. and Ernst, E., 2008. Auricular acupuncture for postoperative pain control: a systematic review of randomised clinical trials. Anaesthesia, 63(12), pp.1343-1348.
- Johnson, R.L. and Wilson, C.G., 2018. A review of vagus nerve stimulation as a therapeutic intervention. Journal of inflammation research, 11, p.203.