Dry Needling, Joint Manipulation, & The Intricate Interconnectivity of the Jaw & Pelvic Floor
Introduction
The trigeminal nerve, cranial nerve V, is an awesome nerve to target with electrical dry needling with the goal of improving autonomic nervous system (ANS) homeostasis. The 3rd branch of the trigeminal nerve, the mandibular branch, and the structures it innervates, are my favorite targets. The 3rd branch of the trigeminal is often referred to as the most parasympathetic-dominant branch. Specifically, I like to needle through the opening just anterior to the TMJ, through the masseters, into the two heads of the lateral pterygoid and the tensor veli palatini. A major trigeminal ganglion, the Otic Ganglion, off which the mandibular branch runs, sits in this space and is an excellent treatment target (not the nerve tissue itself, just close to it).
An odd thing about the trigeminal nerve is it does not seem to have significant efferent autonomic fibers. However, trigeminal afferent fibers travel to the brain stem and project information to extra-trigeminal circuitry in the forebrain, somatosensory cortex, dorsal raphe nucleus, locus coeruleus, hippocampus, and amygdala. Electrical auricular vagus nerve stimulation also regulates these structures. These brain areas have all been demonstrated to play vital roles in regulating the autonomic nervous system toward homeostasis. These connections are thought to be primary mechanisms by which trigeminal nerve stimulation regulates the autonomic nervous system toward homeostasis.
Trigeminal nerve stimulation, like vagus nerve stimulation, has anti-seizure, anti-anxiety, and general calming effects on the nervous systems. Unfortunately, the specific pathways and mechanisms of action are elusive and poorly understood. However, we do understand, we think, an overriding neurophysiologic result secondary to vagus and trigeminal nerve stimulation; sympathetic autonomic depression, parasympathetic autonomic elevation, and ANS homeostasis compared to baseline. Improved autonomic homeostasis helps the body and mind take care of themselves and each other to facilitate and maximize their wonderful, innate healing abilities.
The homeostatic effect on the ANS is amplified with the addition of low frequency (1-5 Hz) microcurrent. I like 1 Hz as it is closest to typical heartbeat. I also like to use binaural auditory beats to amplify the sympathetic depressing effect of my treatments. Delta or Low Delta waves are in this frequency range of 1-5 Hz. This range of frequencies has consistently been shown throughout the literature to amplify the amount of beta endorphins released from the hypothalamic pituitary adrenal (HPA) axis by up to 400%. Beta endorphin is a potent analgesic that reduces pain and sympathetic autonomic hyperactivity. It is also released from numerous white blood cells and plays a role in numerous other poorly understood neurophysiologic mechanisms.
Remember, the overwhelming majority of physical therapy and mental health patients present with chronic sympathetic autonomic hyperactivity. This is one reason treating the mandibular region is so important for a plethora of impairments, especially pelvic floor dysfunction, regardless if there is specific temporomandibular dysfunction or not. Remember, the pelvic floor and the TMJ region are both heavily innervated by the parasympathetic portion of the ANS, which when stimulated, reciprocally inhibits sympathetic activity. The depressive effect stimulating the trigeminal nerve has on sympathetic autonomic activity indicates this treatment will benefit the overwhelming majority of physical therapy patients. This is because the overwhelming majority of physical therapy patients, and humans in general, for that matter, live with chronic sympathetic autonomic hyperactivity. Chronic sympathetic hyperactivity is detrimental to all aspects of health. Achieving a more homeostatic autonomic nervous system will help improve all aspects of mental and physical health. Electrical trigeminal nerve stimulation depresses sympathetic autonomic activity, elevates parasympathetic autonomic activity, and improves autonomic nervous system homeostasis, the key to health.
Embryologically, the urethra, rectum, mouth, and nose are some of the first lumens constructed from our pluripotent sclerotomal cells during early development, and are formed in close proximity to each other. The two locations have striking structural similarities. I hypothesize there is some type of sclerotomal quantum entanglement, or other quantum relationship that takes place upon conception and during embryologic development, forming an intricate relationship between the pelvic floor and jaw that persists throughout life.
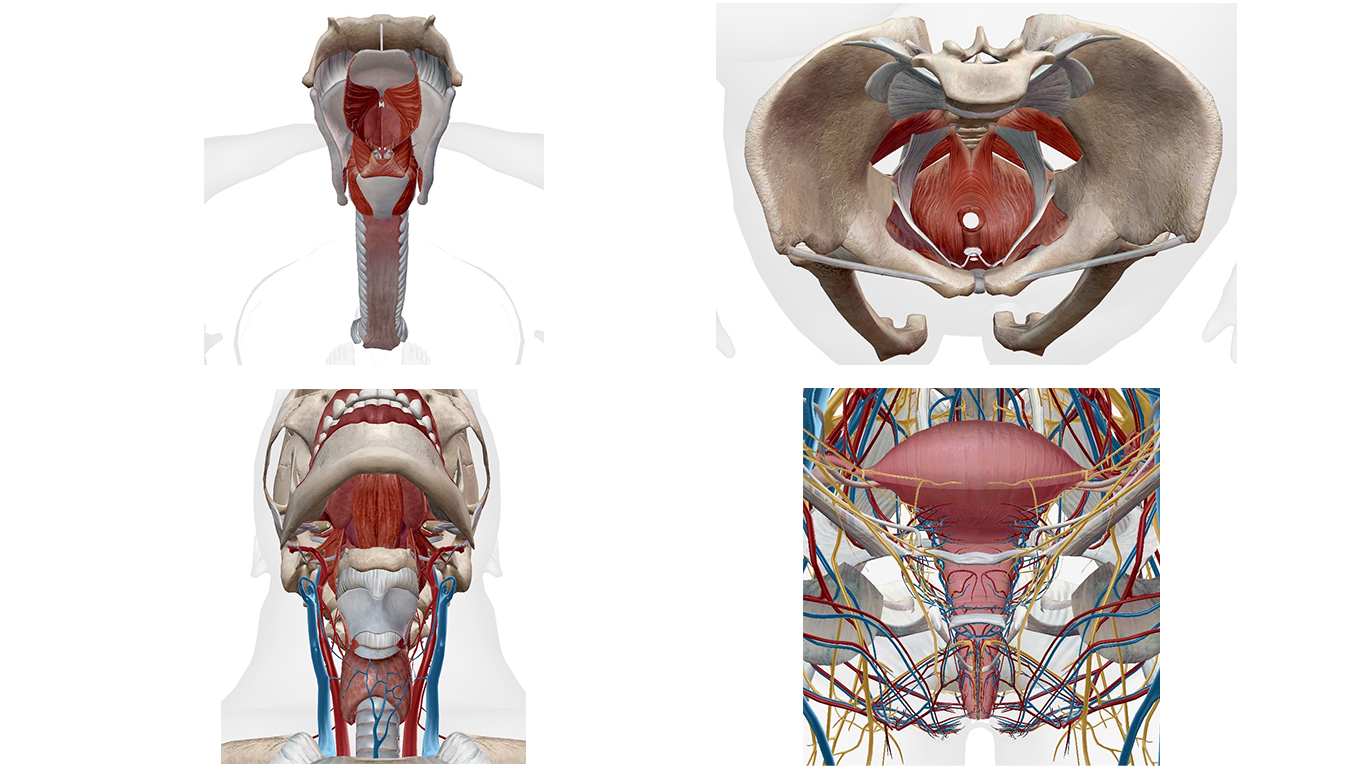
An obvious connection between the jaw and pelvic floor is the fact that both locations are heavily innervated by parasympathetic dominant portions of the autonomic nervous system. The sacral plexus, S2-S4, innervates all 9 pelvic floor muscles, to some degree or other. This is a parasympathetic-dominant portion of the autonomic nervous system, just as the upper cervical spine is, which innervates the mandibular structures via cranial nerves. Since both areas are parasympathetic-dominant, they become reciprocally inhibited secondary to chronic sympathetic hyperactivity. As the sympathetics and parasympathetics reciprocally inhibit each other, the most highly innervated structures by parasympathetic-dominant nerves are typically going to be the most detrimentally affected secondary to sympathetic hyperactivity.

The function of the trigeminocervical complex and trigeminocervical nucleus in the dorsal horn of the cervical spinal cord, both important players in maintaining autonomic homeostasis, are disrupted in instances of chronic sympathetic autonomic hyperactivity. The trigeminocervical nucleus is thought to play a role in cervicogenic dizziness. At the moment, the thought is that enough negative afferents coming from the cervical muscles, whose afferent nerves cross adjacent to the trigeminocervical nucleus, somehow short-circuit the function of this nucleus, leading to autonomic dysregulation. I believe this nucleus, when pathologic, also denigrates pelvic floor function.
In the treatment of almost all physical therapy related impairments, it is vital to stimulate parasympathetics to the maximum extent possible, while at the same time removing as many sympathetic stressors throughout the body as possible, in order to induce autonomic nervous system homeostasis, allowing the mind and body to use their magical, innate abilities to heal themselves and each other. You cannot maximally stimulate parasympathetics without specifically targeting the trigeminal nerve, the vagus nerve, and the sacral plexus.
The temporomandibular region and the pelvic floor are intricately interconnected. To maximize treatment efficacy and outcomes when treating impairments in either area, the other must be concomitantly treated. There are numerous reasons for this, and while many of these reasons remain elusive to our understanding, some obvious connections remain that are somewhat understood. Regardless of the specific mechanistic, correlative aspects of the jaw and pelvic floor, the simple fact of the matter is you will never realize full healing potential without treating them as two parts of a whole.
Thanks for reading. Let me know if anyone has any questions about anything or if you would like to sign up for any of our 4 Dry Needling or 3 manipulation courses. Hosting a course is also a super easy option and the host gets some free spots. Talk to you soon.
Related: Check out our 3 unique certifications
Jason
DISCLAIMER: The content on the blog for Intricate Art Spine & Body Solutions, LLC is for educational and informational purposes only, and is not intended as medical advice. The information contained in this blog should not be used to diagnose, treat or prevent any disease or health illness. Any reliance you place on such information is therefore strictly at your own risk. Please consult with your physician or other qualified healthcare professional before acting on any information presented here.
References
Trigeminal Nerve Stimulation
- Mercante, B., Ginatempo, F., Manca, A., Melis, F., Enrico, P. and Deriu, F., 2018. Anatomo-physiologic basis for auricular stimulation. Medical acupuncture, 30(3), pp.141-150.
- Lauritsen, C.G. and Silberstein, S.D., 2019. Rationale for electrical parameter determination in external trigeminal nerve stimulation (eTNS) for migraine: A narrative review. Cephalalgia, 39(6), pp.750-760.
- McGough, J.J., Sturm, A., Cowen, J., Tung, K., Salgari, G.C., Leuchter, A.F., Cook, I.A., Sugar, C.A. and Loo, S.K., 2019. Double-blind, sham-controlled, pilot study of trigeminal nerve stimulation for attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 58(4), pp.403-411.
- Li, C., White, T.G., Shah, K.A., Chaung, W., Powell, K., Wang, P., Woo, H.H. and Narayan, R.K., 2021. Percutaneous trigeminal nerve stimulation induces cerebral vasodilation in a dose-dependent manner. Neurosurgery, 88(6), pp.E529-E536.
- Stanak, M., Wolf, S., Jagoš, H. and Zebenholzer, K., 2020. The impact of external trigeminal nerve stimulator (e-TNS) on prevention and acute treatment of episodic and chronic migraine: a systematic review. Journal of the Neurological Sciences, 412, p.116725.
- Gil-López, F., Boget, T., Manzanares, I., Donaire, A., Conde-Blanco, E., Baillés, E., Pintor, L., Setoaín, X., Bargalló, N., Navarro, J. and Casanova, J., 2020. External trigeminal nerve stimulation for drug resistant epilepsy: A randomized controlled trial. Brain Stimulation, 13(5), pp.1245-1253.
- Cornelison, L.E., Woodman, S.E. and Durham, P.L., 2020. Inhibition of trigeminal nociception by non-invasive vagus nerve stimulation: investigating the role of GABAergic and serotonergic pathways in a model of episodic migraine. Frontiers in neurology, 11, p.146.
- Henssen, D.J.H.A., Derks, B., van Doorn, M., Verhoogt, N., Van Cappellen van Walsum, A.M., Staats, P. and Vissers, K., 2019. Vagus nerve stimulation for primary headache disorders: An anatomical review to explain a clinical phenomenon. Cephalalgia, 39(9), pp.1180-1194.
- Li, C., Shah, K.A., Powell, K., Wu, Y.C., Chaung, W., Sonti, A.N., White, T.G., Doobay, M., Yang, W.L., Wang, P. and Becker, L.B., 2021. CBF oscillations induced by trigeminal nerve stimulation protect the pericontusional penumbra in traumatic brain injury complicated by hemorrhagic shock. Scientific reports, 11(1), pp.1-15.
Vagus Nerve Stimulation
- Butt, M.F., Albusoda, A., Farmer, A.D. and Aziz, Q., 2020. The anatomical basis for transcutaneous auricular vagus nerve stimulation. Journal of anatomy, 236(4), pp.588-611.
- Garner, B.K., Hopkinson, S.G., Ketz, A.K., Landis, C.A. and Trego, L.L., 2018. Auricular acupuncture for chronic pain and insomnia: a randomized clinical trial. Medical acupuncture, 30(5), pp.262-272.
- Jaić, K.K., Turković, T.M., Pešić, M., Djaković, I., Košec, V. and Košec, A., 2019. Auricular acupuncture as effective pain relief after episiotomy: a randomized controlled pilot study. Archives of gynecology and obstetrics, 300(5), pp.1295-1301
- Johnson, R.L. and Wilson, C.G., 2018. A review of vagus nerve stimulation as a therapeutic intervention. Journal of inflammation research, 11, p.203.
- Kang, H.R., Lee, Y.S., Kim, H.R., Kim, E.J., Kim, K.H., Kim, K.S., Jung, C.Y. and Lee, J.K., 2017. A clinical study of electroacupuncture and auricular acupuncture for abdominal pain relief in patients with pancreatitis: A pilot study. Korean Journal of Acupuncture, 34(1), pp.47-55.
- Moura, C.D.C., Chaves, E.D.C.L., Cardoso, A.C.L.R., Nogueira, D.A., Azevedo, C. and Chianca, T.C.M., 2019. Auricular acupuncture for chronic back pain in adults: a systematic review and metanalysis. Revista da Escola de Enfermagem da USP, 53.
- Sator-Katzenschlager, S.M., Szeles, J.C., Scharbert, G., Michalek-Sauberer, A., Kober, A., Heinze, G. and Kozek-Langenecker, S.A., 2003. Electrical stimulation of auricular acupuncture points is more effective than conventional manual auricular acupuncture in chronic cervical pain: a pilot study. Anesthesia & Analgesia, 97(5), pp.1469-1473.