Dry Needling Combined with Joint Manipulation to Treat & Resolve “Turf Toe:” The Fastest Path to Recovery
Dry Needling Combined with Joint Manipulation to Treat & Resolve “Turf Toe:” The Fastest Path to Recovery
Turf toe is an impairment involving the bottom of your foot at the 1st metatarsophalangeal joint (MTP), the first joint at the base of the big toe.
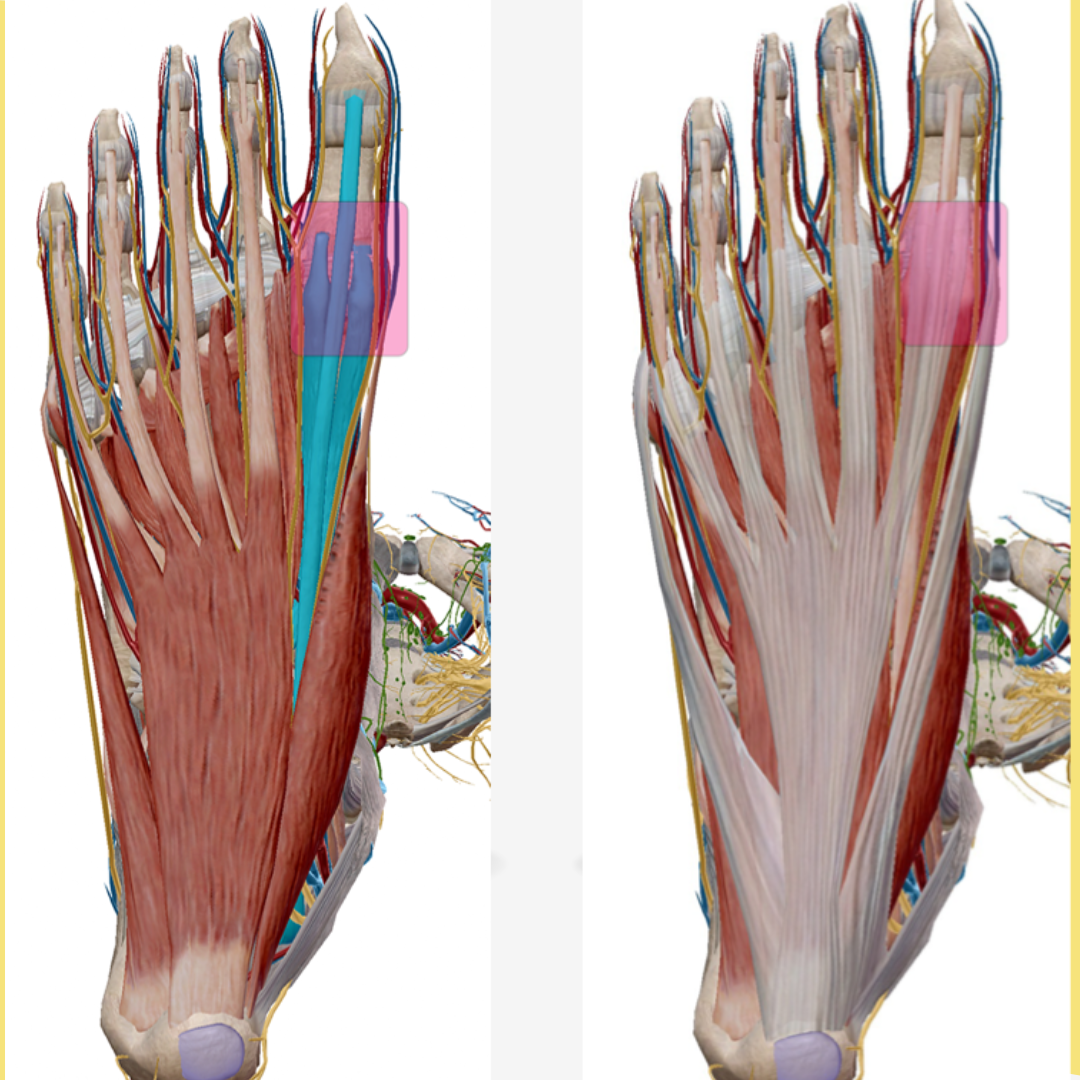
The following structures are typically involved:
- Flexor hallucis longus.
- Flexor hallucis brevis.
- Extensor hallucis longus.
- Extensor hallucis brevis.
- Plantar plate / joint capsule.
- Medial & lateral sesamoid bones.
- 1st Metatarsophalangeal joint (MTP).
The problem may begin suddenly from trauma, like hyperextending the big toe while playing football, or idiopathically, over time, from repeated use. Or from sharks, alligators, snapping turtles, boat motors, drunk fishing guides, you know, the usual stuff. These are all real possibilities when you are a fishing-bum working in South America, trust me… However you hurt your toe, this often turns into a chronic impairment because we rely big-time on our big toes, more than any other toes. It’s also hard to totally rest the bottom of your feet, so there is consistent stress going through the big toes throughout the day, to some degree or other.
The prevalence of turf toe in the NFL has been reported upwards of 10%. That’s like 5-10 players per team that will not perform at optimal level secondary to big toe pain. Not being able to normally stabilize and push through your big toe is a death sentence for any high-level athlete. Soccer, tennis, running, lacrosse, gymnastics, rugby and basketball are all other common sports with frequent turf toe injuries.
Anyway, what I am trying to get at is, turf toe is a common injury, especially when dealing with physically active people. The more physically active and the more stress placed through the feet, the more common the injury. A major problem with turf toe, aside from the fact that it freaking hurts and ruins your ability to do stuff, is that unless you are using needles combined with joint manipulation to treat it, fully resolving turf toe can be something you chase after for an entire professional career, or life, in some cases.
Without Needles, why is turf toe so hard to fix a lot of the time?
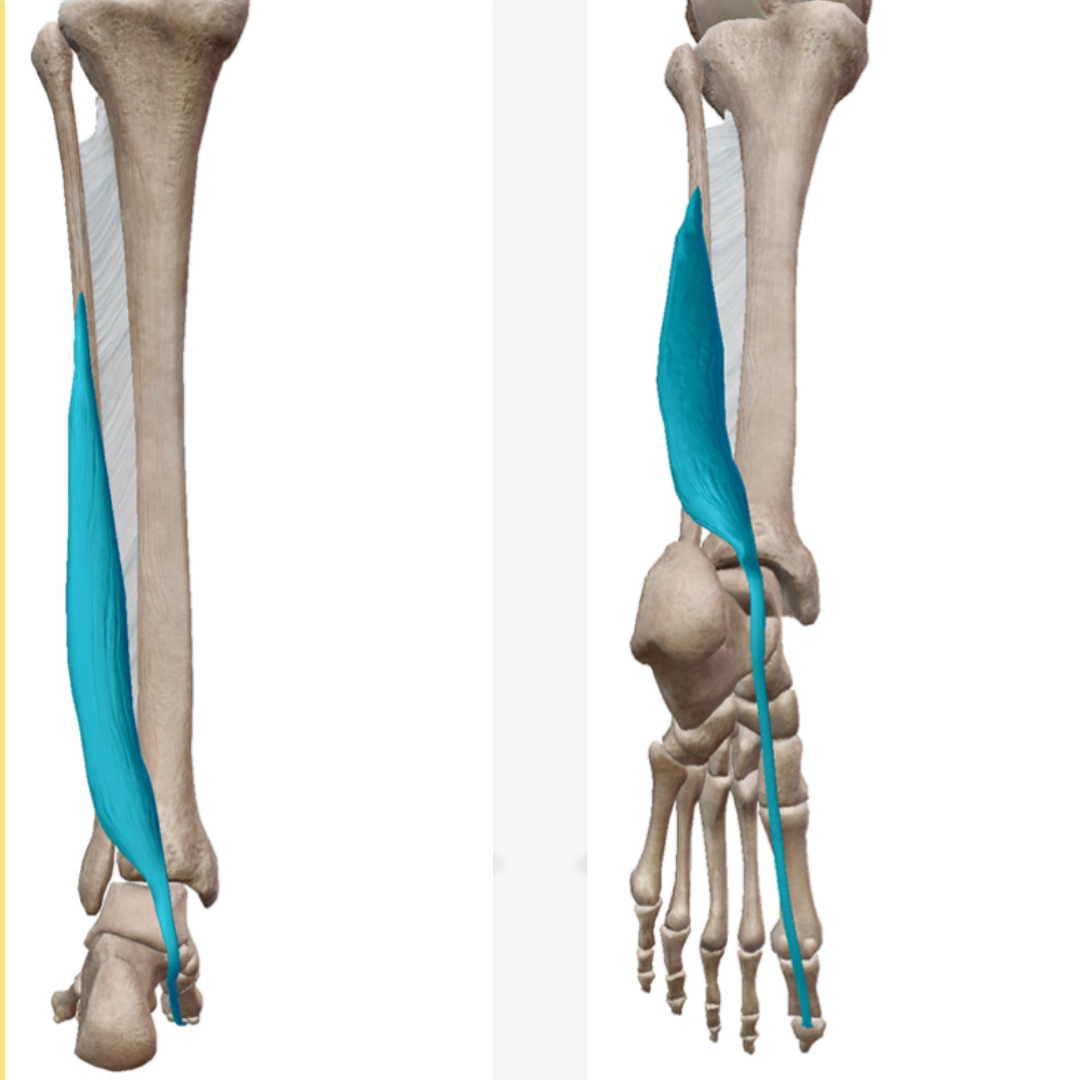
To understand why turf toe sucks so much (that is a medical term), let’s think about the structures involved. The flexor hallucis longus, the biggest big toe flexor and typically the most aggravated contractile tissue in turf toe, is situated in the back of the lateral lower leg. The proximal muscle attachment on the back of the fibula is deep to the soleus and gastroc, and most of the tendon is buried under the plantar fascia and other structures. As with anything but the skin, direct treatment of this muscle is impossible and improvement is often limited, without needles. With needles, it is super easy to treat.
The flexor hallucis brevis is the other muscle crossing the 1st MTP on the bottom. Its proximal attachment, basically right in the middle of the bottom of your foot, is deep to numerous structures; the plantar fascia, flexor digitorum brevis, flexor digitorum longus, and the quadtratus plantae. Again, direct treatment of any muscle or tendon is not possible without needles, and the deeper the structure is, the more indirect the treatment and the worse the response. The extensor hallucis longus and brevis also cross the 1st MTP on the top, but these muscles are typically less involved than the flexors.
Whatever the initial cause of injury, if the condition is chronic, you are going to have periosteal (bone lining) inflammation all around the 1st MTP, along with numerous other locations, including the proximal attachments of the extensor / flexor hallucis longus / brevis. The flexor hallucis longus / brevis (FHL/FHB) are typically the most aggravated contractile tissues crossing the 1st MTP. Once the FHL/FHB are grumpy, they get short. Bastards. They shorten chemically, via excessive acetylcholine release and depressed acetylcholine esterase production, along with the epimysium gaining affinity for acetylcholine. Mechanical shortening occurs via the production of trigger points, hypercontracted groups of skeletal muscle cells (sarcomeres), and joint hypomobility.
Because of the mechanical advantage of the FHL muscle and tendon (lever arm, force arm, bla, bla, bla, I won’t bore you with the specific physics, although it is super cool!), it is capable of producing a huge amount of force. Much more than the FHB. A chronically shorted FHL induces massive joint compression of the 1st MTP. Joint compression is one of the worst possible things to do to any joint. Lucky for us, compression of joints is super easy to fix, if you have needles and manipulation. Otherwise, it can be super tricky.
Once the 1st MTP joint capsule and surrounding structures become inflamed, the joint gets compressed and stops moving through a normal range of motion. The joint capsule is an air / water-tight casing around the joint. The inside of the capsule is made of synovial tissue. The synovial tissue produces synovial fluid (joint oil). However, the synovial tissue only produces adequate fluid if the joint capsule is moved through normal ranges of motion on a consistent basis. If you have turf toe, eating hot, moldy mayonnaise could very well be preferable to really stressing and moving the big toe. This leads to a situation like driving a car with a bunch of old, sandy oil in the engine. Your joint fluid production gets seriously hampered and your joint dries up, loses nutrients, and gets super stiff. This also leads to excessive concentrations of chemicals that become pain amplifiers and inhibit healing. Needling followed by joint manipulation is the best way to resolve this problem.
The importance of targeting the parasympathetic autonomic nervous system (PANS)
Don’t forget where the nerve roots are for the two big toe flexors. The medial plantar nerve, a branch of the tibial nerve, innervates the FHB. The tibial and deep peroneal nerves innervate the FHL. These three nerves all originate from the sciatic nerve, which originates from around L4-S3. S2-S4 is a parasympathetic-dominant portion of the autonomic nervous system (ANS). So, the big toe flexors have a common nerve root origin in the PANS. Therefore, needling the FHL/FHB will stimulate the PANS. This works out awesome for us, as anyone with turf toe is going to be in pain and is going to have sympathetic autonomic nervous system (SANS) hyperactivity. Targeting the PANS depresses SANS hyperactivity, bringing the ANS toward homeostasis. ANS homeostasis is vital to improving all health, including big toe health.
Related: Click here to read a blog on controlling the ANS with DN
You should always target and treat the nerve roots of the distal structures you are treating, and treat bilateral. Doing these two things significantly improves neurologic treatment response and overall treatment efficacy. So, when treating turf toe, it is always good to needle to the lamina of the lumbosacral spine, since that is where the nerves originate. Treating the multifidus and the occipital musculature at C2 spinous process and the base of the occiput, along with the concha of the ears, completes the trifecta of parasympathetic dominant, accessible points of treatment. Treating in this manner dramatically increases patient comfort and treatment efficacy. Don’t forget to use low frequency microcurrent (1-5 Hz).
Remember: the 3 most accessible places to target the PANS with needles are: 1) Concha of the ears (auricular branch, vagus nerve, primary nerve of the PANS). 2) S2-S4. 3) Base of C2 spinous and/or suboccipital periosteum.
Needling is the only direct way to treat inflamed periosteum (bone lining)
Aside from the muscle, tendons and joint capsule we have discussed so far, the periosteum (bone lining), is critically important to address. As with so many other structures, only indirect treatment is available without needles. Indirect treatment is weak! The periosteum is directly accessible with needles. Nice, healthy periosteum feels like a steel plate when you hit it with a needle. It also doesn’t hurt. The more inflamed the periosteum, the mushier it gets and the more it hurts to hit. Poking inflamed periosteum, creating acute inflammation, is one of the ways needling helps tissue heal. New blood and healing nutrients are brought to the area, while the old, nasty, pain-amplifying, growth-inhibiting chemicals that get stuck in the tissues get filtered out. Periosteum also has a much stronger connection to the ANS than does muscle tissue, and needling pathologic periosteum induces stronger homeostatic effects on the ANS, which helps with every medical condition I am aware of.
Once I have needled all the stuff I am going to for that day, I perform my spinal and extremity joint manipulations. Needling prior to joint manipulation makes the manipulation easier, more comfortable, lasting and effective. Remember, joint cavitation, induced by tribonucleation, creates a gas bubble inside the joint capsule. This distracts the joint, removing compression. It is like sticking a little air pump needle into the joint and pumping it up a couple times. Magic.
I do not believe in only addressing the joints in one area of the body, the same way I deal with muscles. For this reason, I address all the tissues and joints in need of a little love, from the tip of the big toe to the top of the head. Needling and manipulation have synergistic effects on the mind and body. Implementing both tools, needling and manipulation, leads to wonderful results that are not otherwise possible.
Related: Click here to learn more about our Manipulation Course offerings
A few other things to think about when treating turf toe
- Don’t forget the muscles traveling from the head that cross the lumbopelvic region. Abnormal tension in these muscles can aggravate the lumbosacral nerve roots, thus aggravating their distal muscle innervations.
- Don’t forget the latissimus, which primarily attaches on the tail bone, humerus, and scapula.
- Ilial anterior rotation will cause a “longer leg,” places most stress on the plantar surface of the 1st MTP. Always address the hips with all impairments.
Thanks for reading everyone. Let me know if anyone has any questions about anything or if you would like to take one of our 7 dry needling and manipulation courses.
Jason
DISCLAIMER: The content on the blog for Intricate Art Spine & Body Solutions, LLC is for educational and informational purposes only, and is not intended as medical advice. The information contained in this blog should not be used to diagnose, treat or prevent any disease or health illness. Any reliance you place on such information is therefore strictly at your own risk. Please consult with your physician or other qualified healthcare professional before acting on any information presented here.
References
Muscle Contraction
- Stojanovic, B., Svicevic, M., Kaplarevic-Malisic, A., Gilbert, R.J. and Mijailovich, S.M., 2020. Multi-scale striated muscle contraction model linking sarcomere length-dependent cross-bridge kinetics to macroscopic deformation. Journal of Computational Science, 39, p.101062.
- Senneff, S. and Lowery, M.M., 2021. Effects of extracellular potassium on calcium handling and force generation in a model of excitation-contraction coupling in skeletal muscle. Journal of Theoretical Biology, 519, p.110656.
- Carter, S. and Solomon, T.P., 2019. In vitro experimental models for examining the skeletal muscle cell biology of exercise: the possibilities, challenges and future developments. Pflügers Archiv-European Journal of Physiology, 471(3), pp.413-429.
- Michailowsky, V., Li, H., Mittra, B., Iyer, S.R., Mazála, D.A.G., Corrotte, M., Wang, Y., Chin, E.R., Lovering, R.M. and Andrews, N.W., 2019. Defects in sarcolemma repair and skeletal muscle function after injury in a mouse model of Niemann-Pick type A/B disease. Skeletal muscle, 9(1), pp.1-15.
- Stern, M.D., Pizarro, G. and Ríos, E., 1997. Local control model of excitation–contraction coupling in skeletal muscle. The Journal of general physiology, 110(4), pp.415-440.
- Rebbeck, R.T., Karunasekara, Y., Board, P.G., Beard, N.A., Casarotto, M.G. and Dulhunty, A.F., 2014. Skeletal muscle excitation–contraction coupling: who are the dancing partners?. The international journal of biochemistry & cell biology, 48, pp.28-38.
- Gong, G., Liu, X. and Wang, W., 2014. Regulation of metabolism in individual mitochondria during excitation–contraction coupling. Journal of molecular and cellular cardiology, 76, pp.235-246.
- Qaisar, R., Bhaskaran, S., Premkumar, P., Ranjit, R., Natarajan, K.S., Ahn, B., Riddle, K., Claflin, D.R., Richardson, A., Brooks, S.V. and Van Remmen, H., 2018. Oxidative stress‐induced dysregulation of excitation–contraction coupling contributes to muscle weakness. Journal of cachexia, sarcopenia and muscle, 9(5), pp.1003-1017.
- Hernández-Ochoa, E.O. and Schneider, M.F., 2018. Voltage sensing mechanism in skeletal muscle excitation-contraction coupling: coming of age or midlife crisis?. Skeletal muscle, 8(1), pp.1-20.
- Squire, J.M., 2016. Muscle contraction: Sliding filament history, sarcomere dynamics and the two Huxleys. Global cardiology science & practice, 2016(2).
- Rassier, D.E., 2017. Sarcomere mechanics in striated muscles: from molecules to sarcomeres to cells. American Journal of Physiology-Cell Physiology, 313(2), pp.C134-C145.
- Powers, J.D., Malingen, S.A., Regnier, M. and Daniel, T.L., 2021. The sliding filament theory since Andrew Huxley: multiscale and multidisciplinary muscle research. Annual review of biophysics, 50, pp.373-400.
- Nishikawa, K., Dutta, S., DuVall, M., Nelson, B., Gage, M.J. and Monroy, J.A., 2020. Calcium-dependent titin–thin filament interactions in muscle: observations and theory. Journal of Muscle Research and Cell Motility, 41(1), pp.125-139.
Autonomic Nervous System
- Li, Q.Q., Shi, G.X., Xu, Q., Wang, J., Liu, C.Z. and Wang, L.P., 2013. Acupuncture effect and central autonomic regulation. Evidence-Based Complementary and Alternative Medicine, 2013.
- Park, S.U., Jung, W.S., Moon, S.K., Park, J.M., Ko, C.N., Cho, K.H., Kim, Y.S. and Bae, H.S., 2008. Effects of acupuncture on autonomic nervous system in normal subjects under mental stress. The Journal of Korean Medicine, 29(2), pp.107-115.
- Haker, E., Egekvist, H. and Bjerring, P., 2000. Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in healthy subjects. Journal of the autonomic nervous system, 79(1), pp.52-59.
- Bäcker, M., Grossman, P., Schneider, J., Michalsen, A., Knoblauch, N., Tan, L., Niggemeyer, C., Linde, K., Melchart, D. and Dobos, G.J., 2008. Acupuncture in migraine: investigation of autonomic effects. The Clinical journal of pain, 24(2), pp.106-115.
- Uchida, C., Waki, H., Minakawa, Y., Tamai, H., Miyazaki, S., Hisajima, T. and Imai, K., 2019. Effects of acupuncture sensations on transient heart rate reduction and autonomic nervous system function during acupuncture stimulation. Medical acupuncture, 31(3), pp.176-184.
- Uchida, C., Waki, H., Minakawa, Y., Tamai, H., Miyazaki, S., Hisajima, T. and Imai, K., 2019. Effects of acupuncture sensations on transient heart rate reduction and autonomic nervous system function during acupuncture stimulation. Medical acupuncture, 31(3), pp.176-184.
- Butts, r., dunning, j. And serafino, c., 2020. Dry needling strategies for musculoskeletal conditions: do the number of needles and needle retention time matter? A narrative review of the literature. Journal of bodywork and movement therapies.
- Castro-Sánchez, A.M., Garcia-López, H., Fernández-Sánchez, M., Perez-Marmol, J.M., Leonard, G., Gaudreault, N., Aguilar-Ferrándiz, M.E. and Matarán-Peñarrocha, G.A., 2020. Benefits of dry needling of myofascial trigger points on autonomic function and photoelectric plethysmography in patients with fibromyalgia syndrome. Acupuncture in Medicine, 38(3), pp.140-149.
- Loaiza, L. A., Yamaguchi, S., Ito, M., & Ohshima, N. (2002). Electro-acupuncture stimulation to muscle afferents in anesthetized rats modulates the blood flow to the knee joint through autonomic reflexes and nitric oxide. Autonomic Neuroscience : Basic & Clinical, 97(2), 103–109. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12132642.
- Morikawa, Y., Takamoto, K., Nishimaru, H., Taguchi, T., Urakawa, S., Sakai, S., … Nishijo, H. (2017). Compression at myofascial trigger point on chronic neck pain provides pain relief through the prefrontal cortex and autonomic nervous system: A pilot study. Frontiers in Neuroscience, 11(APR). https://doi.org/10.3389/fnins.2017.00186.
- Sillevis, R., Van Duijn, J., Shamus, E. and Hard, M., 2021. Time effect for in-situ dry needling on the autonomic nervous system, a pilot study. Physiotherapy theory and practice, 37(7), pp.826-834.
- Lázaro-Navas, I., Lorenzo-Sánchez-Aguilera, C., Pecos-Martín, D., Jiménez-Rejano, J.J., Navarro-Santana, M.J., Fernández-Carnero, J. and Gallego-Izquierdo, T., 2021. Immediate Effects of Dry Needling on the Autonomic Nervous System and Mechanical Hyperalgesia: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(11), p.6018.
- Abbaszadeh-Amirdehi, M., Ansari, N.N., Naghdi, S., Olyaei, G. and Nourbakhsh, M.R., 2017. Therapeutic effects of dry needling in patients with upper trapezius myofascial trigger points. Acupuncture in Medicine, 35(2), pp.85-92.
- Castro-Sánchez, A.M., Garcia-López, H., Fernández-Sánchez, M., Perez-Marmol, J.M., Leonard, G., Gaudreault, N., Aguilar-Ferrándiz, M.E. and Matarán-Peñarrocha, G.A., 2020. Benefits of dry needling of myofascial trigger points on autonomic function and photoelectric plethysmography in patients with fibromyalgia syndrome. Acupuncture in Medicine, 38(3), pp.140-149.
- Skorupska, E., Rychlik, M. and Samborski, W., 2015. Intensive vasodilatation in the sciatic pain area after dry needling. BMC complementary and alternative medicine, 15(1), pp.1-9.
- Clark, N.G., Hill, C.J., Koppenhaver, S.L., Massie, T. and Cleland, J.A., 2021. The effects of dry needling to the thoracolumbar junction multifidi on measures of regional and remote flexibility and pain sensitivity: A randomized controlled trial. Musculoskeletal Science and Practice, 53, p.102366.
- Sánchez-Infante, J., Navarro-Santana, M.J., Bravo-Sánchez, A., Jiménez-Diaz, F. and Abián-Vicén, J., 2021. Is Dry Needling Applied by Physical Therapists Effective for Pain in Musculoskeletal Conditions? A Systematic Review and Meta-Analysis. Physical Therapy, 101(3), p.pzab070.
- Eftekharsadat, B., Babaei-Ghazani, A. and Zeinolabedinzadeh, V., 2016. Dry needling in patients with chronic heel pain due to plantar fasciitis: A single-blinded randomized clinical trial. Medical journal of the Islamic Republic of Iran, 30, p.401.
- Li, Q.Q., Shi, G.X., Xu, Q., Wang, J., Liu, C.Z. and Wang, L.P., 2013. Acupuncture effect and central autonomic regulation. Evidence-Based Complementary and Alternative Medicine, 2013.
- Mori, H., Nishijo, K., Kawamura, H. and Abo, T., 2002. Unique immunomodulation by electro-acupuncture in humans possibly via stimulation of the autonomic nervous system. Neuroscience Letters, 320(1-2), pp.21-24.
- Sakatani, K., Kitagawa, T., Aoyama, N. and Sasaki, M., 2010. Effects of acupuncture on autonomic nervous function and prefrontal cortex activity. In Oxygen Transport to Tissue XXXI (pp. 455-460). Springer, Boston, MA
- Haker, E., Egekvist, H. and Bjerring, P., 2000. Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in healthy subjects. Journal of the autonomic nervous system, 79(1), pp.52-59.
- Shu, Q., Wang, H., Litscher, D., Wu, S., Chen, L., Gaischek, I., Wang, L., He, W., Zhou, H., Litscher, G. and Liang, F., 2016. Acupuncture and moxibustion have different effects on fatigue by regulating the autonomic nervous system: a pilot controlled clinical trial. Scientific reports, 6(1), pp.1-11.
- Matić, Z. and Bojić, T., 2020. Acupuncture, autonomic nervous system and biophysical origin of acupuncture system. Vojnosanitetski pregled, 77(1), pp.79-86.
- Uchida, C., Waki, H., Minakawa, Y., Tamai, H., Hisajima, T. and Imai, K., 2018. Evaluation of autonomic nervous system function using heart rate variability analysis during transient heart rate reduction caused by acupuncture. Medical acupuncture, 30(2), pp.89-95.
- Napadow, V., Beissner, F., Lin, Y., Chae, Y. and Harris, R.E., 2020. Neural Substrates of Acupuncture: From Peripheral to Central Nervous System Mechanisms. Frontiers in neuroscience, 13, p.1419.
- An, S. and Keum, D., 2021. Effect of Acupuncture at the Field of the Auricular Branch of the Vagus Nerve on Autonomic Nervous System Change. Journal of Korean Medicine Rehabilitation, 31(2), pp.81-97.
- Kupari, J. and Ernfors, P., 2020. Pricking into Autonomic Reflex Pathways by Electrical Acupuncture. Neuron, 108(3), pp.395-397.
- Kurita, K., Kiyomitsu, K., Ogasawara, C., Mishima, R., Ogawa-Ochiai, K. and Tsumura, N., 2019. Effect of acupuncture on the autonomic nervous system as evaluated by non-contact heart rate variability measurement. Artificial Life and Robotics, 24(1), pp.19-23.
- Dommerholt, J., Hooks, T., Chou, L.W. and Finnegan, M., 2019. A critical overview of the current myofascial pain literature–November 2018. Journal of bodywork and movement therapies, 23(1), pp.65-73.
- Morikawa, Y., Takamoto, K., Nishimaru, H., Taguchi, T., Urakawa, S., Sakai, S., Ono, T. and Nishijo, H., 2017. Compression at myofascial trigger point on chronic neck pain provides pain relief through the prefrontal cortex and autonomic nervous system: a pilot study. Frontiers in neuroscience, 11, p.186.
- Dommerholt, J., Mayoral, O. and Thorp, J.N., 2021. A critical overview of the current myofascial pain literature–January 2021.
Neural Plasticity
- Dommerholt, J., Mayoral del Moral, O. and Gröbli, C., 2006. Trigger point dry needling. Journal of Manual & Manipulative Therapy, 14(4), pp.70E-87E.
- Calvo, S., Navarro, J., Herrero, P., Del Moral, R., De Diego, C. and Marijuán, P.C., 2015. Electroencephalographic changes after application of dry needling [DNHS© technique] in two patients with chronic stroke. Myopain, 23(3-4), pp.112-117.
- Hsieh, Y.L., Yang, C.C., Liu, S.Y., Chou, L.W. and Hong, C.Z., 2014. Remote dose-dependent effects of dry needling at distant myofascial trigger spots of rabbit skeletal muscles on reduction of substance P levels of proximal muscle and spinal cords. BioMed Research International, 2014.
- Sollie, M., Pind, R., Madsen, C.B. and Sørensen, J.A., 2021. Acupuncture (superficial dry-needling) as a treatment for chronic postherpetic neuralgia–a randomized clinical trial. British Journal of Pain, p.20494637211023075.
- Ren, L., Zhang, W.A., Fang, N.Y. and Wang, J.X., 2008. The influence of electro-acupuncture on neural plasticity in acute cerebral infarction. Neurological research, 30(9), pp.985-989.
- Xiao, L.Y., Wang, X.R., Yang, Y., Yang, J.W., Cao, Y., Ma, S.M., Li, T.R. and Liu, C.Z., 2018. Applications of acupuncture therapy in modulating plasticity of central nervous system. Neuromodulation: Technology at the Neural Interface, 21(8), pp.762-776
- Lo, Y.L., Cui, S.L. and Fook-Chong, S., 2005. The effect of acupuncture on motor cortex excitability and plasticity. Neuroscience letters, 384(1-2), pp.145-149.
- Liu, C.Z., Kong, J. and Wang, K., 2017. Acupuncture therapies and neuroplasticity. Neural plasticity, 2017, p.6178505.
- Li, X. and Wang, Q., 2013. Acupuncture therapy for stroke patients. International review of neurobiology, 111, pp.159-179.
- Kong, J., Gollub, R., Huang, T., Polich, G., Napadow, V., Hui, K., Vangel, M., Rosen, B. and Kaptchuk, T.J., 2007. Acupuncture de qi, from qualitative history to quantitative measurement. The Journal of Alternative and Complementary Medicine, 13(10), pp.1059-1070.
- Lee, J.D., Chon, J.S., Jeong, H.K., Kim, H.J., Yun, M., Kim, D.Y., Kim, D.I., Park, C.I. and Yoo, H.S., 2003. The cerebrovascular response to traditional acupuncture after stroke. Neuroradiology, 45(11), pp.780-784.
- Yang, Y., Eisner, I., Chen, S., Wang, S., Zhang, F. and Wang, L., 2017. Neuroplasticity changes on human motor cortex induced by acupuncture therapy: a preliminary study. Neural plasticity, 2017.
- Jiang, H., Zhang, X., Wang, Y., Zhang, H., Li, J., Yang, X., Zhao, B., Zhang, C., Yu, M., Xu, M. and Yu, Q., 2017. Mechanisms underlying the antidepressant response of acupuncture via PKA/CREB signaling pathway. Neural Plasticity, 2017.
- Tang, H., Guo, Y., Zhao, Y., Wang, S., Wang, J., Li, W., Qin, S., Gong, Y., Fan, W., Chen, Z. and Guo, Y., 2020. Effects and Mechanisms of Acupuncture Combined with Mesenchymal Stem Cell Transplantation on Neural Recovery after Spinal Cord Injury: Progress and Prospects. Neural Plasticity, 2020.
- Lai, H.C., Chang, Q.Y. and Hsieh, C.L., 2019. Signal transduction pathways of acupuncture for treating some nervous system diseases. Evidence-Based Complementary and Alternative Medicine, 2019.
- Pirnia, B., Bazargan, N.M., Hamdieh, M., Pirnia, K., Malekanmehr, P., Maleki, F. and Zahiroddin, A., 2019. The Effectiveness of Auricular Acupuncture on the Levels of Cortisol in a Depressed Patient. Iranian journal of public health, 48(9), pp.1748-1750.
- Yang, J.W., Ye, Y., Wang, X.R., Li, F., Xiao, L.Y., Shi, G.X. and Liu, C.Z., 2017. Acupuncture attenuates renal sympathetic activity and blood pressure via beta-adrenergic receptors in spontaneously hypertensive rats. Neural plasticity, 2017.
- Ye, Y., Zhu, W., Wang, X.R., Yang, J.W., Xiao, L.Y., Liu, Y., Zhang, X. and Liu, C.Z., 2017. Mechanisms of acupuncture on vascular dementia—a review of animal studies. Neurochemistry international, 107, pp.204-210.
- Li, Y., Wang, Y., Liao, C., Huang, W. and Wu, P., 2017. Longitudinal brain functional connectivity changes of the cortical motor-related network in subcortical stroke patients with acupuncture treatment. Neural plasticity, 2017.
- Wang, T., Wu, L., Liao, D., Zhou, X., Chen, Y. and Takeda, A., 2002. Effect of acupuncture on the expression of NT3 in the process of spinal plasticity. Hua xi yi ke da xue xue bao= Journal of West China University of Medical Sciences= Huaxi yike daxue xuebao, 33(1), pp.46-49.
B-endorphin
- Bernstein, H.G., Dobrowolny, H., Bogerts, B., Keilhoff, G. and Steiner, J., 2019. The hypothalamus and neuropsychiatric disorders: psychiatry meets microscopy. Cell and tissue research, 375(1), pp.243-258.
- Roschina, O.V., Levchuk, L.A., Boiko, A.S., Michalitskaya, E.V., Epimakhova, E.V., Losenkov, I.S., Simutkin, G.G., Loonen, A.J., Bokhan, N.A. and Ivanova, S.A., 2021. Beta-Endorphin and Oxytocin in Patients with Alcohol Use Disorder and Comorbid Depression. Journal of Clinical Medicine, 10(23), p.5696.
- Rocchi, G., Sterlini, B., Tardito, S., Inglese, M., Corradi, A., Filaci, G., Amore, M., Magioncalda, P. and Martino, M., 2020. Opioidergic system and functional architecture of intrinsic brain activity: implications for psychiatric disorders. The Neuroscientist, 26(4), pp.343-358.
- Lu, Y., Ann, L. and McCarron, R., 2021. Steroid-induced psychiatric symptoms: What you need to know. Current Psychiatry, 20(4), p.33.
- Maslov, M.Y., Foianini, S., Orlov, M.V., Januzzi, J.L. and Lovich, M.A., 2018. A novel paradigm for sacubitril/valsartan: beta-endorphin elevation as a contributor to exercise tolerance improvement in rats with preexisting heart failure induced by pressure overload. Journal of cardiac failure, 24(11), pp.773-782.
- van der Venne, P., Balint, A., Drews, E., Parzer, P., Resch, F., Koenig, J. and Kaess, M., 2021. Pain sensitivity and plasma beta-endorphin in adolescent non-suicidal self-injury. Journal of Affective Disorders, 278, pp.199-208.
- Furness, J.B., 2000. Types of neurons in the enteric nervous system. Journal of the autonomic nervous system, 81(1-3), pp.87-96.
- McCullough, J.E., Liddle, S.D., Close, C., Sinclair, M. and Hughes, C.M., 2018. Reflexology: a randomised controlled trial investigating the effects on beta-endorphin, cortisol and pregnancy related stress. Complementary therapies in clinical practice, 31, pp.76-84.
- Maslov, M.Y., Foianini, S., Orlov, M.V., Januzzi, J.L. and Lovich, M.A., 2018. A novel paradigm for sacubitril/valsartan: beta-endorphin elevation as a contributor to exercise tolerance improvement in rats with preexisting heart failure induced by pressure overload. Journal of cardiac failure, 24(11), pp.773-782.
- Cui, L., Cai, H., Sun, F., Wang, Y., Qu, Y., Dong, J., Wang, H., Li, J., Qian, C. and Li, J., 2021. Beta-endorphin inhibits the inflammatory response of bovine endometrial cells through δ opioid receptor in vitro. Developmental & Comparative Immunology, 121, p.104074.
Vagus Nerve Stimulation - Sprouse-Blum, A.S., Smith, G., Sugai, D. and Parsa, F.D., 2010. Understanding endorphins and their importance in pain management. Hawaii medical journal, 69(3), p.70.
- Usichenko, T.I., Dinse, M., Hermsen, M., Witstruck, T., Pavlovic, D. and Lehmann, C., 2005. Auricular acupuncture for pain relief after total hip arthroplasty–a randomized controlled study. Pain, 114(3), pp.320-327.
- Usichenko, T.I., Kuchling, S., Witstruck, T., Pavlovic, D., Zach, M., Hofer, A., Merk, H., Lehmann, C. and Wendt, M., 2007. Auricular acupuncture for pain relief after ambulatory knee surgery: a randomized trial. Cmaj, 176(2), pp.179-183.
- Jaić, K.K., Turković, T.M., Pešić, M., Djaković, I., Košec, V. and Košec, A., 2019. Auricular acupuncture as effective pain relief after episiotomy: a randomized controlled pilot study. Archives of gynecology and obstetrics, 300(5), pp.1295-1301
- Taylor, S.L., Giannitrapani, K.F., Ackland, P.E., Thomas, E.R., Federman, D.G., Holliday, J.R., Olson, J., Kligler, B. and Zeliadt, S.B., 2021. The Implementation and Effectiveness of Battlefield Auricular Acupuncture for Pain. Pain Medicine.
- Shah, A.N., Moore, C.B. and Brigger, M.T., 2020. Auricular acupuncture for adult tonsillectomy. The Laryngoscope, 130(8), pp.1907-1912.
- Garner, B.K., Hopkinson, S.G., Ketz, A.K., Landis, C.A. and Trego, L.L., 2018. Auricular acupuncture for chronic pain and insomnia: a randomized clinical trial. Medical acupuncture, 30(5), pp.262-272.
- Kang, H.R., Lee, Y.S., Kim, H.R., Kim, E.J., Kim, K.H., Kim, K.S., Jung, C.Y. and Lee, J.K., 2017. A clinical study of electroacupuncture and auricular acupuncture for abdominal pain relief in patients with pancreatitis: A pilot study. Korean Journal of Acupuncture, 34(1), pp.47-55.
- Moura, C.D.C., Chaves, E.D.C.L., Cardoso, A.C.L.R., Nogueira, D.A., Azevedo, C. and Chianca, T.C.M., 2019. Auricular acupuncture for chronic back pain in adults: a systematic review and metanalysis. Revista da Escola de Enfermagem da USP, 53.
- Tsai, S.L., Fox, L.M., Murakami, M. and Tsung, J.W., 2016. Auricular acupuncture in emergency department treatment of acute pain. Annals of emergency medicine, 68(5), pp.583-585.
- Yeh, C.H., Chiang, Y.C., Hoffman, S.L., Liang, Z., Klem, M.L., Tam, W.W., Chien, L.C. and Suen, L.K.P., 2014. Efficacy of auricular therapy for pain management: a systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine, 2014.
- Sator-Katzenschlager, S.M., Szeles, J.C., Scharbert, G., Michalek-Sauberer, A., Kober, A., Heinze, G. and Kozek-Langenecker, S.A., 2003. Electrical stimulation of auricular acupuncture points is more effective than conventional manual auricular acupuncture in chronic cervical pain: a pilot study. Anesthesia & Analgesia, 97(5), pp.1469-1473.
- Usichenko, T.I., Lehmann, C. and Ernst, E., 2008. Auricular acupuncture for postoperative pain control: a systematic review of randomised clinical trials. Anaesthesia, 63(12), pp.1343-1348.
- Johnson, R.L. and Wilson, C.G., 2018. A review of vagus nerve stimulation as a therapeutic intervention. Journal of inflammation research, 11, p.203.
Orthopedic Conditions
- Clark, N.G., Hill, C.J., Koppenhaver, S.L., Massie, T. and Cleland, J.A., 2021. The effects of dry needling to the thoracolumbar junction multifidi on measures of regional and remote flexibility and pain sensitivity: A randomized controlled trial. Musculoskeletal Science and Practice, 53, p.102366.
- Navarro-Santana, M.J., Gómez-Chiguano, G.F., Cleland, J.A., Arias-Buría, J.L., Fernández-de-Las-Peñas, C. and Plaza-Manzano, G., 2021. Effects of Trigger Point Dry Needling for Nontraumatic Shoulder Pain of Musculoskeletal Origin: A Systematic Review and Meta-Analysis. Physical Therapy, 101(2), p.pzaa216.
- Ma, Y.T., Li, L.H., Han, Q., Wang, X.L., Jia, P.Y., Huang, Q.M. and Zheng, Y.J., 2020. Effects of trigger point dry needling on neuromuscular performance and pain of individuals affected by patellofemoral pain: a randomized controlled trial. Journal of Pain Research, 13, p.1677.
- Carusotto, A.F., Hakim, R.M., Oliveira, R.G., Piranio, A., Coughlan, C.P. and MacDonald, T.J., 2021. Effects of dry needling on muscle spasticity in adults with neurological disorders: a systematic review. Physical Therapy Reviews, pp.1-6.
- Haser, C.H.R.I.S.T.I.A.N., Stöggl, T.H.O.M.A.S., Kriner, M.O.N.I.K.A., Mikoleit, J., Wolfahrt, B., Scherr, J., Halle, M. and Pfab, F., 2017. Effect of dry needling on thigh muscle strength and hip flexion in elite soccer players. Med Sci Sports Exerc, 49(2), pp.378-383.
- Ceballos-Laita, L., Jiménez-del-Barrio, S., Marín-Zurdo, J., Moreno-Calvo, A., Marín-Boné, J., Albarova-Corral, M.I. and Estébanez-de-Miguel, E., 2019. Effects of dry needling in HIP muscles in patients with HIP osteoarthritis: a randomized controlled trial. Musculoskeletal Science and Practice, 43, pp.76-82.
- Geist, K., Bradley, C., Hofman, A., Koester, R., Roche, F., Shields, A., Frierson, E., Rossi, A. and Johanson, M., 2017. Clinical effects of dry needling among asymptomatic individuals with hamstring tightness: a randomized controlled trial. Journal of sport rehabilitation, 26(6), pp.507-517.
- Osborne, N.J. and Gatt, I.T., 2010. Management of shoulder injuries using dry needling in elite volleyball players. Acupuncture in medicine, 28(1), pp.42-45.
- Albin, S.R., Koppenhaver, S.L., MacDonald, C.W., Capoccia, S., Ngo, D., Phippen, S., Pineda, R., Wendlandt, A. and Hoffman, L.R., 2020. The effect of dry needling on gastrocnemius muscle stiffness and strength in participants with latent trigger points. Journal of Electromyography and Kinesiology, 55, p.102479.
- Navarro-Santana, M.J., Sanchez-Infante, J., Gómez-Chiguano, G.F., Cleland, J.A., López-de-Uralde-Villanueva, I., Fernández-de-Las-Peñas, C. and Plaza-Manzano, G., 2020. Effects of trigger point dry needling on lateral epicondylalgia of musculoskeletal origin: a systematic review and meta-analysis. Clinical Rehabilitation, 34(11), pp.1327-1340.
- Segura-Ortí, E., Prades-Vergara, S., Manzaneda-Piña, L., Valero-Martínez, R. and Polo-Traverso, J.A., 2016. Trigger point dry needling versus strain–counterstrain technique for upper trapezius myofascial trigger points: a randomised controlled trial. Acupuncture in Medicine, 34(3), pp.171-177.
- Charles, D., Hudgins, T., MacNaughton, J., Newman, E., Tan, J. and Wigger, M., 2019. A systematic review of manual therapy techniques, dry cupping and dry needling in the reduction of myofascial pain and myofascial trigger points. Journal of bodywork and movement therapies, 23(3), pp.539-546.
- Mullins, J.F., Nitz, A.J. and Hoch, M.C., 2021. Dry needling equilibration theory: A mechanistic explanation for enhancing sensorimotor function in individuals with chronic ankle instability. Physiotherapy theory and practice, 37(6), pp.672-681.
- Cagnie, B., Castelein, B., Pollie, F., Steelant, L., Verhoeyen, H. and Cools, A., 2015. Evidence for the use of ischemic compression and dry needling in the management of trigger points of the upper trapezius in patients with neck pain: a systematic review. American journal of physical medicine & rehabilitation, 94(7), pp.573-583.
- Sánchez-Infante, J., Bravo-Sánchez, A., Jiménez, F. and Abián-Vicén, J., 2021. Effects of Dry Needling on Muscle Stiffness in Latent Myofascial Trigger Points: A Randomized Controlled Trial. The Journal of Pain.
- Alaei, P., Ansari, N.N., Naghdi, S., Fakhari, Z., Komesh, S. and Dommerholt, J., 2020. Dry Needling for Hamstring Flexibility: A Single-Blind Randomized Controlled Trial. Journal of Sport Rehabilitation, 30(3), pp.452-457.
- Dommerholt, J., 2011. Dry needling—peripheral and central considerations. Journal of Manual & Manipulative Therapy, 19(4), pp.223-227.
- Tough, E.A., White, A.R., Cummings, T.M., Richards, S.H. and Campbell, J.L., 2009. Acupuncture and dry needling in the management of myofascial trigger point pain: a systematic review and meta-analysis of randomised controlled trials. European Journal of Pain, 13(1), pp.3-10.
- Ansari, N.N., Alaei, P., Naghdi, S., Fakhari, Z., Komesh, S. and Dommerholt, J., 2020. Immediate effects of dry needling as a novel strategy for hamstring flexibility: a single-blinded clinical pilot study. Journal of sport rehabilitation, 29(2), pp.156-161.
- Mason, J.S., Crowell, M., Dolbeer, J., Morris, J., Terry, A., Koppenhaver, S. and Goss, D.L., 2016. The effectiveness of dry needling and stretching vs. stretching alone on hamstring flexibility in patients with knee pain: a randomized controlled trial. International journal of sports physical therapy, 11(5), p.672s.
DISCLAIMER: The content on the blog for Intricate Art Spine & Body Solutions, LLC is for educational and informational purposes only, and is not intended as medical advice. The information contained in this blog should not be used to diagnose, treat or prevent any disease or health illness. Any reliance you place on such information is therefore strictly at your own risk. Please consult with your physician or other qualified healthcare professional before acting on any information presented here.
Stay Engaged With Intricate Art
Get the latest news, updates and offers from Intricate Art delivered to your inbox.